Franklin Building Supply strives to provide a balanced, comprehensive benefits program for their employees. The Franklin Building Supply Employee Benefits program offers you core benefits, such as Medical and Dental as well as voluntary Vision, Life, and Disability benefits that help maximize your coverage options. This booklet is designed to help you understand your coverage, premiums and options for this year. This is a reference for you and your family to make informed insurance decisions based on your specific needs. The official plan documents will always govern.
HEALTHCARE CONCIERGE
Touchcare Healthcare Assistance Services | (866) 486-8242 | touchcare.com | assist@touchcare.com
Who is TouchCare?
TouchCare is your personal health assistant. We’re here to provide free, confidential assistance to help take the stress out of healthcare. Let us help find in-network doctors, get cost estimates, deal with billing issues and explain your benefits...all at no cost to you.
Here’s how we can help you:
- Answer benefit questions in plain language
- Fix billing errors and review medical claims
- Provider searches and appointment scheduling
- Provide cost estimates for upcoming procedures
Call (866) 486-8242 for quick answer to your questions!

ELIGIBILITY
HOW TO ENROLL
Using your desktop or mobile device, you have access to our online benefits enrollment platform 24/7. In your Paylocity portal you can:
- View and select benefits for yourself and dependents
- View per-pay-period amounts
- Submit qualifying events
- Add and edit beneficiaries and dependents
To get started, click on the link below to head to your enrollment portal!
IMPORTANT: Current participants must complete their enrollment in Paylocity to continue participating in the FSAs. Enrollment does NOT carry forward year to year. There is a fee of $1.75 per pay period to participate.
QUALIFYING LIFE EVENTS
Under certain circumstances, employees may be allowed to make changes to benefit elections during the plan year, if the event affects the employee, spouse, or dependent’s coverage eligibility. Any requested changes must be consistent with and on account of the qualifying event.
Examples Of Qualifying Events:
- Legal marital status (for example, marriage, divorce, legal separation, annulment);
- Number of eligible dependents (for example, birth, death, adoption, placement for adoption);
- Work schedule (for example, full-time, part-time);
- You, your spouse, or other covered dependent become enrolled in Part A, Part B, or Part D of Medicare
- Death of a spouse or child;
- Change in your child’s eligibility for benefits (reaching the age limit);
- Becoming eligible for Medicaid; or
- Your coverage or the coverage of your Spouse or other eligible dependent under a Medicaid plan or state Children’s Health Insurance Program (“CHIP”) is terminated as a result of loss of eligibility and you request coverage under this Plan no later than 60 days after the date the Medicaid or CHIP coverage terminates; or
- You, your spouse or other eligible dependent become eligible for a premium assistance subsidy in this Plan under a Medicaid plan or state CHIP (including any waiver or demonstration project) and you request coverage under this Plan no later than 60 days after the date you are determined to be eligible for such assistance.

MEDICAL
Customer Service | (888) 675-6570 | www.regence.com
NETWORK: Regence BlueShield of Idaho Preferred Network
How do I find an In-Network Provider?
- Use the helpful link below! In-Network providers can also be found on your provider’s website at www.regence.com under “Find Care”. Select "Find a Doctor" and then you can search by provider/facility name or search by specialty. You can also use the link below.
- To get the most benefit from your plan, you should use network providers. The BlueCross BlueShield PPO network is available to you wherever you are. The website and customer service phone numbers are located on the back of your Medical ID card. Register as a member on www.regence.com to review your claims, get benefit information, and to access valuable tools for members only.
Did You Know?
- Preventive Services are covered at 100% In-Network and copays & deductibles do not apply.
- You pay less out of pocket if you receive care from an In-Network provider.
- You do not need to designate a primary care physician or need a referral to see a Specialist.
Below is an overview of the medical plan offered by Franklin Building Supply.
Looking for more details about how items are covered? Please refer to the formal Summary of Benefits and Coverage (SBC) below.
PHARMACY
Franklin Building Supply has selected OptumRx as your backend claims manager, giving you access to one of the largest national pharmacy networks. OptumRx’s web portal and app will help you manage your medications anywhere, anytime, search for the nearest retail pharmacy, and check drug interactions
A Formulary Drug List specifies which drugs are covered under your prescription drug benefit. How much you pay out of pocket is determined by whether your drug is on the list and at what coverage level, or tier. A generic drug is often at the lower tier. See if your drug is covered by reviewing your formulary drug list using the link below.
Sign-Up for Mail Order Pharmacy:
- Get up to a three-month supply of your maintenance medication(s) delivered safely and reliably right to your door. Save time and money!
ID Cards:
- Your permanent ID card(s) will be distributed to you shortly by your medical vendor. If you need to fill a prescription before your card(s) arrives, simply provide all of the information on the card below to the pharmacy to process your request.
If there are any questions regarding prescription coverage, please contact RxBenefits Member Services team at (800)-334-8134 available Monday - Friday from 7 am to 8 pm CT or by emailing them at CustomerCare@rxbenefits.com.
With Virtual Visits, the doctor is always in. Get 24/7 non-emergency care from a board-certified doctor by phone, online video or mobile app from the privacy and comfort of your own home. Don’t risk crowded waiting rooms, expensive urgent care or ER bills, or waiting weeks or more to see a doctor, when you can speak with a Virtual Visits doctor within minutes.
Virtual Visits, provided by your Regence Medical Plan and powered by MDLIVE®, are a convenient alternative for treatment of more than 80 health conditions, including allergies, cold, flu, fever, headaches, nausea, sinus infections, etc.
Virtual Visits with licensed behavioral health therapists are available by appointment. Get virtual care for anxiety, depression, stress management, and more.
YOU PAY $0 PER CONSULT
Get Started
Set Up Account
- Visit www.MDLIVE.com/regence-id and click on "ACTIVATE NOW" to complete the required information to set up your account.
Provide Your Information
- You will need to provide your Regence Subscriber ID# and fill out the required fields to continue.
- Phone: MDLIVE can help you complete your information over the phone. Call (888) 680-8646.
Request a Consult
- Once your account is set up, request a consult anytime you need care

FLEXIBLE SPENDINGS ACCOUNT (FSA)
Customer Service | (800) 274-0503 | www.nbsbenefits.com
A Flexible Spending Account is an indispensable part of your overall benefits program. An FSA is an account your employer sets up so you can pay for a variety of healthcare needs, like insurance co-pays, deductibles, dental, vision, pharmacy and even some over-the-counter medication costs, reimbursed under the Health FSA. But here’s the best part: Your FSA is funded entirely by your pre-tax income. This means you can save money and offset rising healthcare costs at the same time. That’s like found money to spend on all those everyday items you and your family need!
Why Participate?
- FSAs save you money! The contributions you make to an FSA are deducted from your pay check on a pre-tax basis – before federal income, social security, and most state taxes. FSAs help you:
- Reduce taxable income – Contributions lower your reported annual income, resulting in lower taxable wages.
- Save on healthcare expenses – Using pre-tax funds to pay out of pocket expenses can save you hundreds!
- Offset rising healthcare costs and individual financial responsibility.
Maximum Annual Contribution
- For the 2026 plan year, the Health Care FSA allows you to set aside up to $3,400 pre-tax money to pay for a variety of qualified medical, dental, vision, and pharmacy expenses.
- Annual contribution amounts you elect for the plan year must be set during enrollment and can not be changed except for changes in family status.
Rollover Benefit
- For the 2026 plan year, up to $680 of your unused funds will rollover to the 2027 plan year. Any additional remaining funds will be forfeited.
- You must submit your claims by March 31st of the following year.
Eligible Expenses
- A full list of qualified FSA expenses can be found in IRS Publication 502 at www.irs.gov.
- You can learn more about FSA qualified expenses and also make purchases by visiting the FSA Store at www.fsastore.com.
IMPORTANT: Current participants must complete their enrollment in Paylocity to continue participating in the FSAs. Enrollment does NOT carry forward year to year. There is a fee of $1.75 per pay period to participate.

DEPENDENT CARE FSA (DCA)
Customer Service | (800) 274-0503 | www.nbsbenefits.com
A Dependent Care FSA (DCA) is a reimbursement program that allows employees (participants) to set aside pre-tax funds to help pay for qualified dependent care expenses. Most participants use this program to pay for child daycare and after-school care expenses; however, it can be used to pay for adult daycare expenses as well. It serves as an alternative to using the Dependent Care Tax Credit. Funds can only be used on a dependent child under the age of 13 or dependents who are unable to care for themselves. Unlike a Flexible Spending Account, DCA funds can only be used as they are deposited into your account.
Why Participate?
- Tax Savings! Child and dependent care is a large expense for many American families. Millions of people rely on childcare to be able to work, while others are responsible for older parents or disabled family members. If you pay for care of dependents in order to work, you’ll want to consider taking advantage of the savings this plan offers. Money contributed to a DCA is free from federal income, Social Security, and Medicare taxes and remains tax-free when it is spent.
Maximum Annual Contribution
- For the 2026 plan year, you can contribute up to $7,500 ($3,500 if married and filing separately).
- This is a "use it as you accrue it" account.
Eligible Expenses
- You may be reimbursed only for care that enables you to work, go to school full-time, or look for work on a full-time basis. DCA funds can be used on expenses such as tuition for licensed daycare facility, preschool, after-school programs, elder care, summer day camps, in-home dependent care services, and more.
Visit your FSA Member Portal to check your account balance, file new claims, set up direct deposit, check the status of a claim, and much more.
NOTE: The Health Care FSA is independent of the Dependent Care FSA and you cannot transfer funds between accounts.

HEALTH MARKETS
Are you in the market for Medicare?
Maybe you’re looking down the road toward your 65th birthday, and you’re pretty sure that after that point, you are entitled to Medicare benefits ... but you have some questions. At HealthMarkets, we realize changes to Medicare and the general complexity associated with health insurance can become overwhelming. That’s why we want to provide you with the most accurate information on Medicare so that you can make an informed decision about your health coverage.
At HealthMarkets Insurance Agency, we can help you get the insurance coverage you need whenever, and however, you want to shop for it:
- In Person Assistance: With 3,000+ licensed, knowledgeable agents and more than 200 offices and retail locations across the country, you can meet with an agent face to face to learn about your insurance options.
- Just a Phone Call Away: Personalized assistance and counsel is available over the phone 24/7 allowing you to shop for insurance when it’s most convenient for you.
- Do It Yourself Convenience: As a certified web broker with the Federal Government, we provide a broad array of health insurance related topics and plans, including a selection of price and benefit options through a user friendly shopping experience for those who prefer to explore their options online.
HINGE HEALTH
Hinge Health through Regence is an online physical therapy source for people with Musculoskeletal pain. At Hinge they offer a unique approach to pain management by not only giving you a physical therapist to work with but also a dedicated support coach who will assist you with the pressures and issues outside of just physical pain. Hinge believes that having a complete care team is imperative to keeping people consistent and engaged with their exercises. They really want people to feel that they have an easy access point to physical therapy,
For a person negatively affected by their environment, being healthy can be difficult. Environmental factors such as poor access to healthy food, lack of safe sidewalks, and limited access to public transit inhibit good habits
Here's how it works:
- Tell us about yourself:
- Complete a 10-minute questionnaire to open your account and tell us about your experience with pain. Once your account is approved, you can log into the app.
- Help us build a care plan
- Download the Hinge Health app and log in to your account. Then, do a few exercises so we can learn about your pain. This allows us to design the right care plan to help you do more every day, with less pain.
- Start your Program
- And start feeling better! As your pain improves, so does your care plan—with new exercises and tools to help you move with confidence.
Get Started by using the app!
DENTAL
Franklin Building Supply offers you two dental programs: Delta Dental and Willamette Dental. The two plans operate very differently. For example, the Delta Dental plan pays a percentage of covered services up to an annual maximum whereas the Willamette plan has no annual maximum and you pay a set fee for covered services. Learn more about each of the plans in the sections below.
Customer Service | (888) 899-3734 | www.deltadental.com
NETWORK: Delta Dental PPO Plus Premier Network
How do I find a Delta Dental In-Network Dentist?
- Click the link below or visit www.deltadentalid.com and select “Find a Dentist” wherever you are located or you may contact customer service at (208) 489-3580.
- You have the freedom to select the dentist of your choice; however, when you visit a participating in-network dentist, you will have lower out-of-pocket costs, no balance billing, and claims will be submitted by your dentist on your behalf.
Pre-treatment Estimate
- If your dental care is extensive and you want to plan ahead for the cost, you can ask your dentist to submit a pre-treatment estimate. While it is not a guarantee of payment, a pre-treatment estimate can help you predict your out-of-pocket costs.
Dental Health Education and Online Risk Assessment Tool
- Delta Dental provides an Oral Health and Wellness site that includes an interactive risk assessment tool that will assess your risk of dental disease. Any member can access a vast array of wellness topics, articles and the interactive risk assessment. Click the link below to learn more.
Discount Orthodontia – Only available in Idaho
- Members can receive a discounted fee for adult and child orthodontia when you obtain care from an orthodontist that participates in the Discount Program. For program details and a list of participating providers, click the link below.
Looking for more details about how items are covered? Click on the link below to view the formal Benefit Summary

Customer Service | (855) 433-6825 | www.willamettedental.com
NETWORK: Willamette Dental
How do I find a Willamette In-Network Dentist?
- Click the link below or visit www.willamettedental.com or you may contact member services at (855) 433-6825.
- You have the freedom to select the dentist of your choice; however, when you visit a participating in-network dentist, you will have lower out-of-pocket costs, no balance billing, and claims will be submitted by your dentist on your behalf.
IMPORTANT: The Willamette clinic locations are ideal for employees who live in the Boise or Twin Falls areas. If you live outside these areas, please consider the proximity to your nearest clinic before signing up for this coverage option.
What to Expect at Your First Visit
- During your first visit, you’ll receive a thorough dental exam that includes X-rays and a comprehensive risk assessment. Your dentist will develop a Proactive Dental Care Plan based on your current and long-term oral health goals. The plan will include recommendations for cleanings, restorations and preventive treatments.

VISION
Customer Service | (888) 581-3648 | www.eyemed.com
NETWORK: Insight Network
How do I find an In-Network Provider?
- Click the link below or visit www.eyemed.com and select "Find an Eye Doctor" under the "Members and Consumers" tab.
- You may also contact member services at (866) 804-0982. For LASIK, call (800) 988-4221.
Did You Know?
- Eyes can give doctors a clear picture of overall wellness. That’s why vision care—and vision benefits—can help employees stay healthy. A comprehensive eye exam can detect early signs of serious health problems, such as diabetes, heart disease, high blood pressure, high cholesterol, glaucoma and cataracts
Additional Benefits
- The vision plan offers additional benefits such as:
- 40% off additional complete pair of prescription eyeglasses
- 20% off non-covered items, including non-prescription sungless
- Hearing Care from Aplifon Network - Up to 64% off hearing aids
- LASIK or PRK from U.S. Laser Network - 15% off retail or 5% off promo price
- Log into eyemed.com/member to see all plans included with your benefits!
Looking for more details about how items are covered? Click on the link below to view the formal Benefit Summary.

LIFE & AD&D
Customer Service | (800) 657-6351 | www.unitedheritage.com
Franklin Building Supply offers group Voluntary Term Life and Accidental Death and Dismemberment insurance for you and Voluntary Term Life for your dependents through United Heritage. This option gives you the advantage of purchasing life insurance coverage at affordable group rates.
Guaranteed Issue Amount
- If you enroll within 30 days of becoming eligible, you qualify for the Guaranteed Issue amount. This means you are eligible to elect up to this amount without having to provide proof of good health.
- Employee – up to $150,000
- Spouse – up to $50,000
- Children – up to $10,000
How much coverage can I buy?
- Employee – $10,000 increments, not to exceed the lesser of 5 times your salary or $500,000 with matching AD&D coverage
- Spouse – $5,000 increments up to $100,000 (the spouse benefit cannot exceed 50% of employee’s benefit)
- Children – $2,000 increments up to $10,000 from 6 months up to age 26 (birth to 6 months benefit is $1,000)
- Keep in mind that your benefit will reduce to 65% at age 70, to 45% at age 75, to 30% at age 80, to 20% at age 85, to 15% at age 90 & over.
- The percentage reduction is based on original coverage prior to any reductions at each policy anniversary.
- An EOI is required for any change in coverage amounts.

PORTABILITY & CONVERSION
Life insurance portability and conversion options are features that allow policyholders to maintain some level of insurance coverage when they might otherwise lose it or wish to change the type of coverage they have.
Portability
- Refers to the ability of an individual to transfer their group life insurance coverage from one employer to another or from a group policy to an individual policy without undergoing new underwriting or providing evidence of insurability.
- This is commonly associated with group term life insurance provided by employers. If you (the employee) leave your job or retire, you may not want to lose your life insurance coverage, especially if there are ongoing health issues. Advantages of porting coverage are that it allows continuity of coverage and there is no need for medical examination or evidence of insurability.
- The application and check for the initial premium must be received within 31 days after Life Insurance terminates or 15 days from the date the Employer signs the application; whichever is later.
Conversion
- The Conversion option allow you to convert your term life insurance policy into permanent (e.g., whole life or universal life) insurance policy without providing evidence of insurability or undergoing new underwriting. Transitions from term to permanent coverage without having to do a new medical exam.
- This option is considered when an individual has ongoing health issues or may be unable to qualify for a new policy.
- An Insured Employee and Dependent(s) may convert Group Voluntary Life Insurance coverage, without evidence of insurability, to an Individual Life Insurance policy during the 31 day period following termination of employment.
It's essential for policyholders to consider the options available to you and request conversion or portability timely, within 30 days of your benefits termination. You will submit the request for conversion or portability directly to the insurance carrier and will set up direct payment for your new individual policy.
DISABILITY

Customer Service | (800) 657-6351 | www.unitedheritage.com
Voluntary Short-Term Disability
Have you considered how a sickness, pregnancy or accidental injury may prevent you from working for more than a few days? Financially, how might that affect you? Could you afford to pay for gas or your rent or mortgage for a few months if something were to happen?
Franklin Building Supply has provided you the opportunity to enroll in a Short Term Disability program that will provide you the financial protection you may need. This benefit replaces a portion of the income you may lose when afflicted by a disability. It’s like paycheck insurance
- Coverage Amount - Covers 60% of your weekly income, up to a maximum benefit of $1,200 per week.
- Elimination Period - Benefits begin on the 8th day of an injury or illness.
- Benefit Duration - Payments may last up to 12 weeks (You must be sick or disabled for the duration of the waiting period before you can receive a benefit payment).
- Pre-existing Condition Exclusion - No treatment for the condition for 180 days or insured for 365 consecutive days; a pre-existing condition is treatment an employee received within 90 days before the effective date

Voluntary Long-Term Disability
Franklin Building Supply has provided you the opportunity to enroll in a Long Term Disability program that will provide you the financial protection you may need.mThis voluntary coverage pays a monthly benefit if you have a covered illness or injury and you can't work for a few months - or even longer! You're generally considered disabled if you're unable to do important parts of your job - and your income suffers as a result.
- Coverage Amount - Covers 60% of your monthly income, up to a maximum benefit of $5,000 per month.
- Elimination Period - Benefits begin on the 91st day of an injury or illness (STD pays during this period)
- Benefit Duration
- If you elect Option 1 and you become disabled prior to age 63, benefits will be paid to normal Social Security retirement age (SSNRA).
- If you elect Option 2 and you become disabled prior to age 61, benefits will be paid for up to 60 months only
- Pre-existing Condition Exclusion - No treatment for the condition for 180 days or insured for 365 consecutive days; a pre-existing condition is treatment an employee received within 90 days before the effective date
Personal issues, planning for life events or simply managing daily life can affect your work, health and family. ComPsych® DisabilityGuidance provides support, resources and information for personal and work-life issues. DisabilityGuidance is company-sponsored, confidential and provided at no charge to you and your dependents. The flyer below explains how DisabilityGuidance can help you and your family deal with everyday challenges.
Confidential Counseling
- This no-cost counseling service helps you address stress, relationship and other personal issues you and your family may face. It is staffed by Guidance Consultants—highly trained master’s and doctoral level clinicians who will listen to your concerns and quickly refer you to in-person counseling and other resources.
Financial Information and Resources
- Speak by phone with our Certified Public Accountants and Certified Financial Planners on a wide range of financial issues.
- GuidanceResources Online is your one stop for expert information on the issues that matter most to you... relationships, work, school, children, wellness, legal, financial, free time and more
NOTE: Before a disability claim, DisabilityGuidance offers insured Policyholders up to five sessions per calendar year. Following an approved LTD Claim, claimants are also entitled to five additional sessions. The sessions may be used with a counselor, financial planner or lawyer or split among the three types of professionals.
ANYTIME EXTRA BENEFITS
InsurChoice offers you the ability to personalize your protection program — bringing you quick, convenient, holistic coverage with incredible cost-saving discounts across a variety of top-rated insurance products and carriers. Our program is simple, fast, and always online. Find coverage in the blink of an eye!
Key benefits include:
- Competitive pricing: One size doesn’t fit all, so you can match yourself with the best rates and coverages from multiple insurance companies.
- Custom-tailored coverage: Select the products that meet YOUR needs.
- Stability: We have relationships with key national carriers who have a proven track record of rate and coverage stability.
- Innovation: With our innovative product delivery platform we are constantly striving to add more benefits and improve your experience.
Click the link below to receive your FREE no obligation quote customized especially for you!
EMPLOYEE ASSISTANCE PROGRAM (EAP)
Find professional support when you need it for challenging life events.
- ComPsych GuidanceResources is an Employee Assistance Program (EAP) included with your LTD United Heritage plan.
- You and your family members can use EAP services — no copays or deductibles needed.
Reach Out
Don’t be afraid to reach out for help. Your health records are kept private from your employer, as required by law.
- Call: (866) 511-3361
- TDD: (800) 697-0353
- Online: guidanceresources.com
- App: GuidanceNow
- Web ID: EAP4UH
OTHER BENEFITS
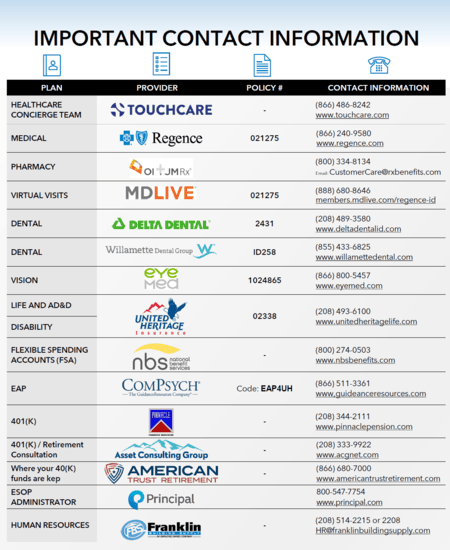
CONTACT INFO
FREQUENTLY ASKED QUESTIONS (FAQs)
Why go to an In-network provider?
- Going to an in-network provider means choosing a healthcare professional or facility that has a contract with your health insurance plan. In-network providers have agreed to offer their services at negotiated rates, which are often lower than what you would pay for out-of-network care. By visiting an in-network provider, you can take advantage of your health insurance plan's benefits, which may include lower copayments, coinsurance, and reduced out-of-pocket expenses.
Why should I go for my annual well checkup?
- Annual well checkups are essential for maintaining good health and preventing potential health issues. These visits allow your doctor to assess your overall health, monitor any chronic conditions you might have, and detect early signs of potential health problems. Regular checkups help identify health concerns before they become serious, ensuring timely intervention and a better chance for successful treatment.
What is the difference between generic and brand name drugs?
- Generic drugs are identical or bioequivalent to brand-name drugs in terms of active ingredients, safety, strength, dosage form, and intended use. The main difference is that generic drugs are usually more affordable because they don't have the research and development costs associated with brand-name drugs. The U.S. Food and Drug Administration (FDA) ensures that generic drugs meet the same rigorous standards for quality, safety, and effectiveness as their brand-name counterparts.
How do discount cards work on RX?
- Prescription discount cards provide discounts on medications at participating pharmacies. These cards are often available for free or at a low cost and can be used by individuals without insurance or those with high copayments. When you present the discount card at the pharmacy, it reduces the price of the medication, potentially leading to significant cost savings.
What happens if I go out of network?
- If you go out of network for healthcare services, it means you're seeing a provider or using a facility that doesn't have a contract with your health insurance plan. Out-of-network care typically results in higher out-of-pocket costs, including higher copayments, coinsurance, and potentially higher deductibles. Some health insurance plans may not cover out-of-network care at all, except in emergencies.
What is a SBC (Summary of Benefits and Coverage)?
- A Summary of Benefits and Coverage (SBC) is a document provided by health insurance companies to help individuals understand their health plan's key features and coverage details. It provides a summary of the plan's benefits, costs, coverage limits, and examples of common medical scenarios to help individuals compare different health insurance options and make informed decisions.
What is an EOB (Explanation of Benefits)?
- An Explanation of Benefits (EOB) is a statement sent by the health insurance company to the policyholder after a healthcare claim has been processed. The EOB provides a detailed explanation of the services provided, the amount billed by the healthcare provider, the amount covered by the insurance, and any remaining balance that the insured may be responsible for paying.
What should I ask my doctor?
- When visiting your doctor, consider asking questions related to your health condition, treatment options, medications, potential side effects, and any lifestyle changes you should make. You can also inquire about preventive measures, recommended screenings, and follow-up care. Don't hesitate to ask for clarification if there's anything you don't understand.
What is preventive care?
- Preventive care refers to healthcare services aimed at preventing or detecting health issues before they become more severe or chronic. Examples of preventive care include vaccinations, screenings (e.g., mammograms, colonoscopies), regular checkups, counseling on healthy behaviors, and interventions to manage risk factors.
Where can I get my ID card?
- You can typically get your health insurance ID card from your insurance provider. Many insurers offer electronic versions of the ID card through their mobile apps or member portals. Alternatively, you can request a physical ID card to be mailed to you.
Who do I contact if I have a QLE (Qualifying Life Event)?
- If you experience a Qualifying Life Event (QLE), such as marriage, birth/adoption of a child, divorce, loss of other health coverage, or a change in household income, you should contact your employer's HR department or your health insurance provider promptly. They can guide you through the process of updating your health insurance coverage or enrolling in a new plan if necessary.