Table of Content
- Header
-
Open Enrollment
- ALEX: YOUR VIRTUAL BENEFITS COUNSELOR
- HOW TO ENROLL
- PLAN ELIGIBILITY
- QUALIFYING LIFE EVENTS
- MEDICAL
- MEDICAL PLAN OPTIONS
- MEDICAL PLAN COSTS
- Summary of Benefits and Coverage (SBC)
- EXTRAS FROM BCBS
- PHARMACY
- Drug Card
- HEALTH SAVINGS ACCOUNT (HSA)
- DENTAL
- DENTAL PLAN OPTIONS
- DENTAL PLAN COSTS
- VISION
- VISION PLAN
- VISION PLAN COSTS
- LIFE AND AD&D
- SHORT-TERM DISABILITY (STD)
- EMPLOYEE ASSISTANCE PROGRAM (EAP)
- PET INSURANCE
- CONTACT US
- REQUIRED NOTICES
- Footer
HOW TO ENROLL
Using your desktop or mobile, you have access to our online benefits enrollment platform 24/7. In your Paycom portal you can:
- View and select benefits for yourself and dependents
- View per-pay-period amounts
- Submit qualifying events
- Add and edit beneficiaries and dependents
Download the Paycom Mobile App from Google Play or the App Store to get started or click on the link below to head to your enrollment portal!
IMPORTANT: The Benefit choices you make during your initial enrollment or annual open enrollment remain in effect for the entire plan year unless you experience a qualifying life event.

PLAN ELIGIBILITY
EMPLOYEE ELIGIBILITY
Regular full-time employees and employees working 130 hours per month or more are eligible to participate in the benefit plans. Coverage for full-time employees will be effective 1st of the month following 60 days from your date of hire. Hours worked for variable hour employees will be tracked for a set measurement period to determine benefits eligibility and effective date.
DEPENDENT ELIGIBILITY
You may also enroll eligible dependents for benefits coverage. A ‘dependent’ is defined as the legal spouse/domestic partner and ‘dependent child(ren)’ of the plan participant or the spouse.
The term ‘child’ refers to any of the following:
A natural (biological) child;
A stepchild;
A legally adopted child;
A foster child;
A child for whom legal guardianship has been awarded to the participant or the participant’s spouse/domestic partner; or
Disabled dependents may be eligible if requirements set by the plan are met.
QUALIFYING LIFE EVENTS
Your premiums for medical, dental, and vision insurance are deducted on a pre-tax basis through a Cafeteria Plan established under Section 125 of the Internal Revenue Code (IRC). Under Section 125, changes to an employee's pre-tax benefits can only be made during the Open Enrollment period unless the employee or qualified dependents experience a qualifying event and the request to make a change is made within 30 days of the qualifying event.
Under certain circumstances, employees may be allowed to make changes to benefit elections during the plan year, if the event affects the employee, spouse, or dependent’s coverage eligibility. Any requested changes must be consistent with and on account of the qualifying event.
Examples Of Qualifying Events:
- Legal marital status (for example, marriage, divorce, legal separation, annulment);
- Number of eligible dependents (for example, birth, death, adoption, placement for adoption);
- Work schedule (for example, full-time, part-time);
- You, your spouse, or other covered dependent become enrolled in Part A, Part B, or Part D of Medicare
- Death of a spouse or child
- Change in your child’s eligibility for benefits (reaching the age limit);
- Becoming eligible for Medicaid; or
- Your coverage or the coverage of your Spouse or other eligible dependent under a Medicaid plan or state Children’s Health Insurance Program (“CHIP”) is terminated as a result of loss of eligibility and you request coverage under this Plan no later than 60 days after the date the Medicaid or CHIP coverage terminates; or
- You, your spouse or other eligible dependent become eligible for a premium assistance subsidy in this Plan under a Medicaid plan or state CHIP (including any waiver or demonstration project) and you request coverage under this Plan no later than 60 days after the date you are determined to be eligible for such assistance.
IMPORTANT: If you experience any of these qualifying life events during the year, be sure to reach out to your HR Department within 30 days to make changes to your benefit elections. If you miss that special enrollment window, you will have to wait until the next open enrollment period to make changes.
MEDICAL
NETWORK: BlueChoice PPO
How do I find an In-Network Provider? Use the helpful link below!
- In-Network providers can also be found on your provider’s website at www.bcbstx.com under “Find Care”. Select "Find a Doctor or Hospital" and then you can search by provider/facility name or search by specialty.
Did You Know?
- Preventive Services are covered at 100% In-Network and copays & deductibles do not apply.
- You pay less out of pocket if you receive care from an In-Network provider.
- You do not need a referral to see a Specialist.
You have 2 medical plans to choose from. Compare the options in the chart below!
MEDICAL PLAN COSTS
Summary of Benefits and Coverage (SBC)
Looking for more details about how items are covered? Please refer to the formal Summary of Benefits and Coverage (SBC) below. There is one for each plan!
EXTRAS FROM BCBS
As a BCBS member, you have access to a plethora of services and resources!
This is only a brief description of some of the plan benefits. For more complete details, including benefits, limitations and exclusions, please login to your BAM portal.
Blue Access for Members (BAM)
Through Blue Access for Members (BAM), you can access health plan information, resources and tools. The information can vary, depending on your plan.
- Review benefits, account balances, claims status and more.
- Order a replacement ID card or print a temporary card.
- View and print an Explanation of Benefits (EOB) for a claim.
Blue Access Mobile
Blue Access Mobile makes it easy for you to access your information while on the go. You can view coverage details, health and wellness information, check claim status and access member ID card information. You can also sign up to get text or email alerts and tips
Valuable Member Programs
As a BCBSTX member, you have access to a range of programs that can help you get and stay healthy.
- Health and wellbeing programs can help you manage your health conditions, get pregnancy support, talk to a nurse 24/7 and more.
- Blue365® offers discounts on health-related products, health and fitness clubs, weight-loss programs and much more.
PHARMACY
Prescription drugs are a vital part of your health care coverage. If you have prescription drug coverage through Blue Cross and Blue Shield of Texas (BCBSTX), this information can help you and your doctor get the most from your prescription drug coverage. The Pharmacy Benefit Manager for BCBS is Prime Therapeutics. You can access more information about your pharmacy coverage by visiting www.myprime.com.
A drug list is a list of drugs that are covered under your prescription drug benefit. How much you pay out of pocket is determined by whether your drug is on the list and at what coverage level, or tier. A generic drug is often at the lower tier. See if your drug is covered by reviewing your formulary drug list using the link below!
Express Scripts® Pharmacy, the mail order pharmacy for members with BCBSTX prescription drug coverage, provides safe, fast and cost-effective pharmacy services that can save you time and money. With this program, you can obtain up to a 90-day supply of long-term (or maintenance) medications through Express Scripts® Pharmacy.
Ordering Through Express Scripts® Pharmacy
Getting Started Online
You have more than one option to fill or refill a prescription online or from a mobile device:
- Visit express-scripts.com/rx Follow the instructions to register and create a profile.
- Log in to myprime.com and follow the links to Express Scripts® Pharmacy.
Order Over the Phone
Call 1-833-715-0942, 24/7, to refill, transfer a current prescription or get started with home delivery. Please have your member ID card, prescription information and your doctor’s contact information available.
Review your prescription costs for each plan in the chart below!
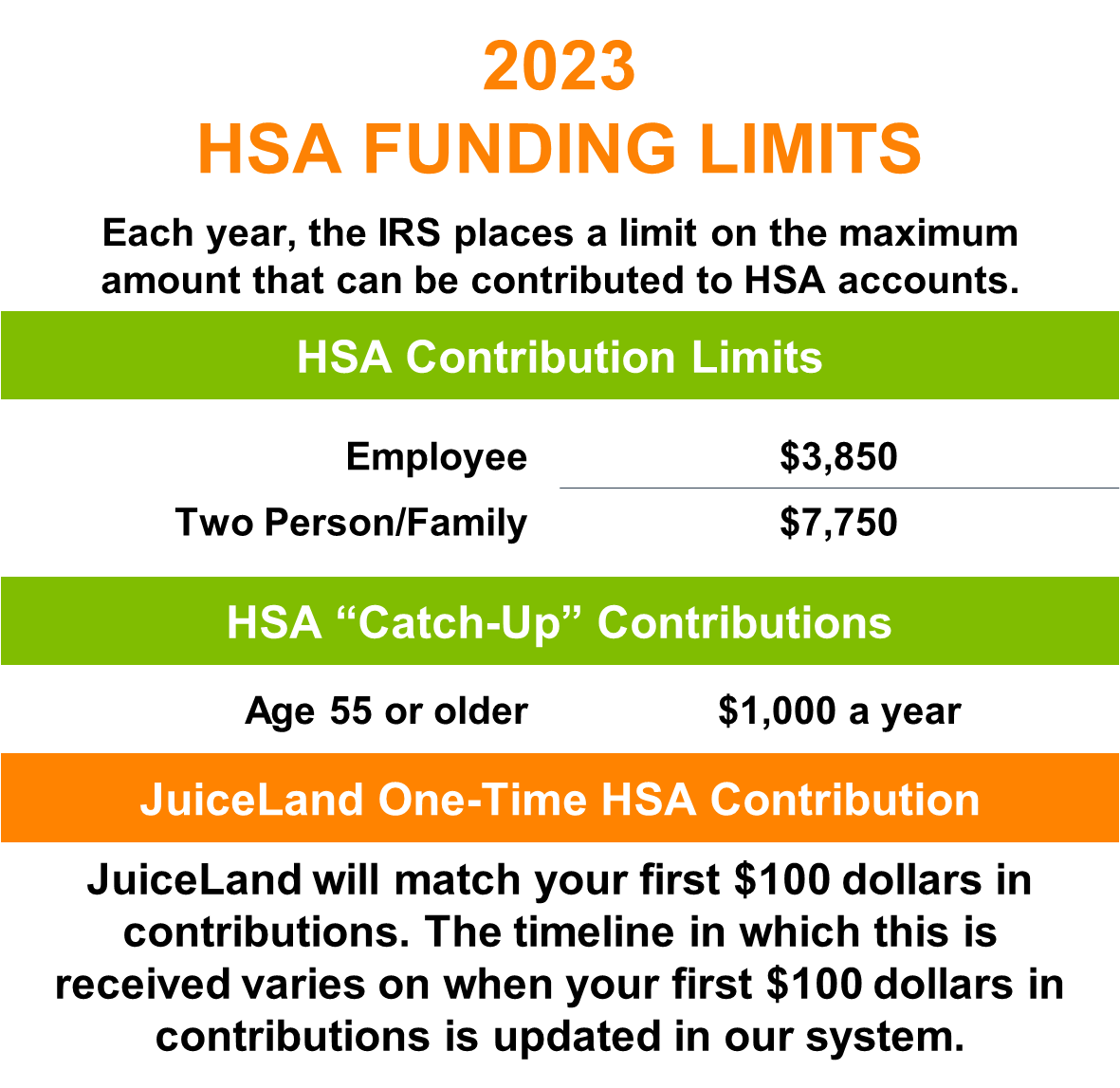
HEALTH SAVINGS ACCOUNT (HSA)
A Health Savings Account (HSA) is a tax-free savings account owned by you and lets you build up savings for future approved medical expenses. The funds may be used to pay for qualifying healthcare expenses for yourself, your spouse or dependents. You decide how much you would like to contribute, when and how to spend the money on eligible expenses, and how to invest the balance. Go to www.healthequity.com to learn more.
UNDERSTANDING YOUR HSA
- Pre-tax contributions are deducted through payroll and deposited into your HSA account.
- You can use your HSA available funds to pay for qualified medical expenses tax-free
- HSA funds used for non-eligible expenses will be subject to regular income taxes and a 20% excise tax penalty.
- Unused funds remain in your account for future use and roll over each calendar year
- An HSA remains with you even if you change health plans or companies. If you open an HSA and later become ineligible to make contributions, you can still use your remaining funds
- You can change your HSA contribution at any time during the plan year for any reason
DENTAL
NETWORK: Principal Plan Dental Network
How do I find an In-Network Provider? Use the helpful link below!
- In-Network providers can also be found on your provider’s website at www.principal.com by clicking "Find a dentist".
Did You Know?
- You have the freedom to select the dentist of your choice; however, when you visit a participating in-network dentist, you will have lower out-of-pocket costs, no balance billing, and claims will be submitted by your dentist on your behalf.
Pre-treatment Estimate
- If your dental care is extensive and you want to plan ahead for the cost, you can ask your dentist to submit a pre-treatment estimate. While it is not a guarantee of payment, a pre-treatment estimate can help you predict your out-of-pocket costs.
Looking for more details about how items are covered? Click on the link below to view the formal Benefit Summary.
A summary of your dental benefits is shown in the chart below!
DENTAL PLAN COSTS
VISION
NETWORK: VSP Choice
How do I find an In-Network Provider? Use the helpful link below!
- In-Network providers can also be found on your provider’s website at www.vsp.com or by calling 1 (800) 877-7195
Did You Know?
Eyes can give doctors a clear picture of overall wellness. That’s why vision care—and vision benefits—can help employees stay healthy. A comprehensive eye exam can detect early signs of serious health problems, such as:
- Diabetes
- Heart disease
- High blood pressure
- High cholesterol
- Glaucoma and cataracts
Looking for more details about how items are covered? Click on the link below to view the formal Benefit Summary.
A summary of your vision benefits is shown in the chart below!
VISION PLAN COSTS
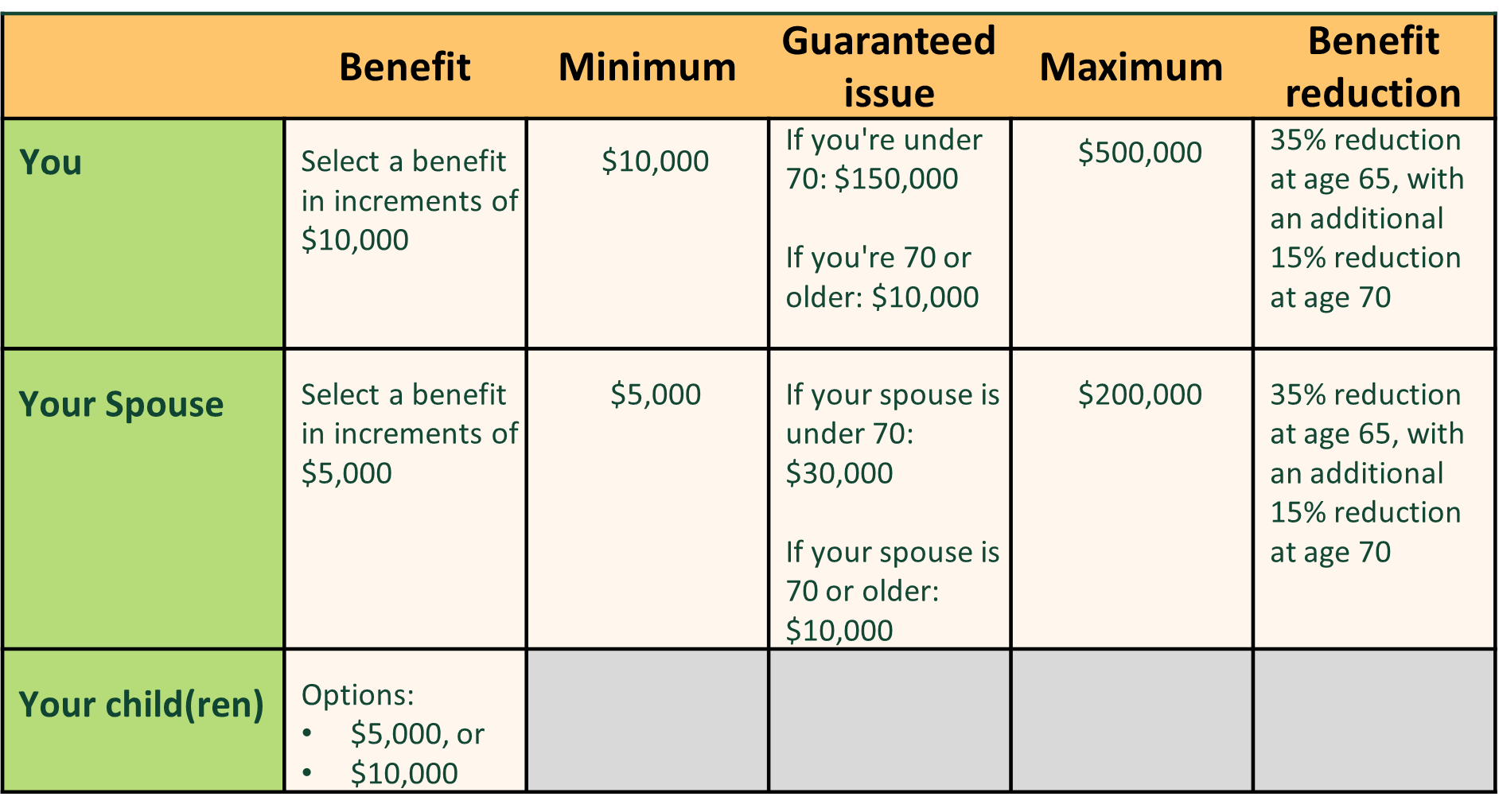
LIFE AND AD&D
Life insurance coverage is your opportunity to provide for and protect the people you love most. By putting a plan in place to cover expenses that would occur in the event of your death, you can help secure their long-term financial future. Your coverage needs depend on factors such as your age, your financial strength, and your family’s circumstances. In general, the earlier you are in life and the more financially dependent your loved ones are on you, the more coverage you need.
Through your employer, you have the opportunity to enroll in Voluntary Life insurance with Accidental Death & Dismemberment (AD&D) coverage. Coverage is also available for your spouse and/or child dependents, however, it is required that you elect coverage for yourself in order to elect coverage for your dependents. See the grid to the right for the plan specifics!
Guarantee Issue (GI) Benefit
When you are first eligible (at hire) for Voluntary Life and AD&D, you may purchase up to the Guaranteed Issue (GI) for yourself and your spouse without providing proof of good health.
Any amount elected over the GI benefit will require Evidence of Insurability (EOI). If you elect voluntary life coverage and are required to complete an EOI form, it is your responsibility to complete and return it to the insurance carrier. In addition, your spouse will need to provide EOI to be eligible for coverage amounts over GI, or if coverage is requested at a later date.
Online Evidence of Insurability (EOI)
If you elect an amount of coverage that will require you to complete an EOI form, you will receive an email from Principal with instructions on how to complete the form online. Create an account on the carrier website by registering as a member and follow the instructions to complete your health statement. After submitting, you will either receive auto approval or notification that additional health information is needed. If more information is needed, you will receive a letter with details.
Annual Increase During Open Enrollment
Open enrollment is a great time to increase your coverage. You can add an additional $20,000 in coverage for yourself - with no health questions asked. If you have coverage for yourself, you can also add or increase coverage for your spouse and children without medical questions. During open enrollment, you and/or your spouse can request to add or increase even more coverage by completing an Evidence of Insurability form.
SHORT-TERM DISABILITY (STD)
Everyday illnesses or injuries can interfere with your ability to work. Even a few weeks away from work can make it difficult to manage household costs. Your employer-paid Short Term Disability coverage provides financial protection for you by paying a portion of your income, so you can focus on getting better and worry less about keeping up with your bills.
Benefit Amount: 60% of your weekly salary up to $1,000 per week
Elimination Period: Benefits begin after the 14th day calendar day
Maximum Benefit Period: Benefits will continue until the employee returns to work or has been disabled for up to 11 weeks; whichever occurs first.
EMPLOYEE ASSISTANCE PROGRAM (EAP)
Have something on your mind and need to talk with someone who understands? We’ve got you covered! Get the support you’re looking for through your Employee Assistance Program (EAP).
Our support is confidential, free of cost, and available 24/7, 365 days a week.
Your EAP is designed to help you lead a happier and more productive life at home and at work. Call for confidential access to a Licensed Professional Counselor who can help you with:
Go to login.lifeworks.com or call (800) 433-7916
Username: JuiceLand / Password: lifeworks
PET INSURANCE
Give your best friend their best life with Wishbone Pet Health Insurance!
Wishbone offers high-value, easy-to-use pet health insurance at exclusive employee benefit rates. Get reimbursed for vet bills that resulted from an accident or illness with your pet. Coverage includes diagnostics and testing, unexpected surgery, hospitalization, emergency care, hereditary and congenital conditions, and more.
With Wishbone, you get:
· 90% reimbursement on accidents and illnesses
· A low $250 annual deductible
· Fast claims processing
· Visit any licensed veterinarian
· Easy-to-use member account
· And so much more!
Plus, choose from two tiers of optional routine care add-ons to maximize your savings on everyday pet care.
Submit a claim from your account online. Claims are processed within five business days, and you'll receive fast reimbursement payouts via check or direct deposit. Wishbone includes a durable ID tag with lost pet recovery service and 24/7 pet telehealth support for each insured pet.
REQUIRED NOTICES
Federal regulations require employers to provide certain notifications and disclosures to all eligible employees. The booklet linked below is dedicated to those disclosures for 1/1/2023 – 12/31/2023. If you have any questions or concerns, please contact your HR Department.
If you (and/or your dependents) have Medicare or will become eligible for Medicare in the next 12 months, a federal law gives you more choices about your prescription drug coverage. Please see page 4 of the Required Notices packet for more information about your options.