Table of Content
- Header
-
ENROLLMENT
- HOW TO ENROLL
- QUALIFYING LIFE EVENTS
-
MEDICAL & PRESCRIPTION
- MEDICAL SUMMARY
- SUMMARY OF BENEFITS AND COVERAGE (SBC)
- PRESCRIPTIONS
- PRESCRIPTION SUMMARY
- VIRTUAL VISITS
-
ANTHEM SERVICES
- DOWNLOAD ANTHEM'S SYDNEY HEALTH APP
- HOW TO FIND IN-NETWORK PROVIDERS
- 24/7 NURSELINE
- ANTHEM ID CARD
-
DELTA DENTAL
- Dental Plan
-
VISION
- VISION SUMMARY
-
BASIC LIFE AND VOLUNTARY LIFE
- BENEFICIARY DESIGNATION
- GUARANTEED ISSUE (GI)
-
LONG-TERM DISABILITY
- DISABILITY SUMMARY
-
Spending Accounts
- Health Savings Account (HSA)
- Flexible Spending (FSA) & Dependent Care Accounts (DCARE)
- Health Reimbursement Account (HRA)
-
RESOURCES
- MEDICARE ELIGIBLITY
- GLOSSARY
- REQUIRED NOTICES
- FREQUENTLY ASKED QUESTIONS (FAQs)
- Footer
WELCOME TO YOUR VIRTUAL BENEFITS GUIDE!
It’s that time of year—our Open Enrollment period is right around the corner!
This is your opportunity to review, select, and make any necessary changes to your benefits for the upcoming year. We want to make sure you have all the information you need, so here’s a quick rundown:
KEY INFORMATION TO KNOW:
When is Open Enrollment?
- Open Enrollment period:
- This is the only time you can make changes to your benefits outside of a qualifying life event.
What’s Changing?
What’s Staying the Same?
Reminder: If satisfied with current insurance/benefit choices above and you have no changes, we still highly recommend reviewing everything to ensure your choices and personal information are still accurate.
HOW TO ENROLL
ENROLLMENT INSTRUCTIONS
- Sign into Paylocity. You can access the Paylocity website through SharePoint or the link below!
- Click HR & Payroll in the top left corner.
- Click Bswift Benefits.
- Click "Start Your Enrollment".
QUALIFYING LIFE EVENTS
Under certain circumstances, employees may be allowed to make changes to benefit elections during the plan year, if the event affects the employee, spouse, or dependent’s coverage eligibility. Any requested changes must be consistent with and on account of the qualifying event.
Examples Of Qualifying Events:
- Legal marital status (for example, marriage, divorce, legal separation, annulment);
- Number of eligible dependents (for example, birth, death, adoption, placement for adoption);
- Work schedule (for example, full-time, part-time);
- You, your spouse, or other covered dependent become enrolled in Part A, Part B, or Part D of Medicare
- Death of a spouse or child;
- Change in your child’s eligibility for benefits (reaching the age limit);
- Becoming eligible for Medicaid; or
- Your coverage or the coverage of your Spouse or other eligible dependent under a Medicaid plan or state Children’s Health Insurance Program (“CHIP”) is terminated as a result of loss of eligibility and you request coverage under this Plan no later than 60 days after the date the Medicaid or CHIP coverage terminates; or
- You, your spouse or other eligible dependent become eligible for a premium assistance subsidy in this Plan under a Medicaid plan or state CHIP (including any waiver or demonstration project) and you request coverage under this Plan no later than 60 days after the date you are determined to be eligible for such assistance.

MEDICAL & PRESCRIPTION
The Directions Group offers a medical plan through Anthem.
A PPO option offers the freedom to see any provider when you need care. When you use providers from within the PPO network, you receive benefits at the discounted network cost. Most expenses, such as office visits, emergency room, and prescription drugs are covered by a copay. Other expenses are subject to a deductible and coinsurance. The HDHP is similar to the PPO Plan in that you have the option to choose any provider when you need care. However, in exchange for a lower per-paycheck cost, you must satisfy a higher deductible that applies to almost all health care expenses, including those for prescription drugs. All expenses are your responsibility until the deductible is reached, with the exception of preventive care, which is covered at 100% when you visit a physician in the network. Once the deductible is met, you are responsible for coinsurance for medical expenses and a copay for prescription drug expenses. An HMO gives you access to doctors and hospitals within the HMO network. But unlike PPO plans, care under an HMO plan is covered only if you see a provider within that HMO’s network.
Utilizing In-Network providers will allow for the highest level of coverage. In-Network providers agree to accept Anthem contract rate as the final charge and the member is not balanced billed.
Medical Summary
Looking for more details about how items are covered? Please refer to the formal Summary of Benefits and Coverage (SBC) below.
PRESCRIPTIONS
TRADITIONAL DRUGS
TIER 1 (GENERIC) | Lowest copay: Most drugs in this category are generic drugs. Members pay the lowest copay for generics, making these drugs the most cost-effective option for treatment.
TIER 2 | Low copay: This category includes non-preferred and low-cost generic drugs
TIER 3 | Higher copay: This category includes preferred, brand-name drugs that don't yet have a generic equivalent. These drugs are more expensive than generics, and have a higher copay.
TIER 4 | Highest copay: In this category are nonpreferred brand name drugs for which there is either a generic alternative or a more cost-effective preferred brand including most specialty medications. These drugs have the highest copay. Make sure to check for mail-order discounts that may be available.
Helpful Rx Cost Savings Tools & Tips:
MAIL ORDER - Many drugs are available in a 90-day supply, rather than the 30-day retail supply. Typically, you will pay less if you choose to get a mail-order 90-day supply.
GOOD Rx - There are many tools online that you can use to save on prescription costs. One is GoodRx.com, an online Rx database that allows you to find what pharmacy is the cheapest for your specific prescription. Additionally, you may be able to find a coupon that will greatly reduce your cost. It is important to remember that many of the coupons can only be used outside of your plan (which will not count towards your maximums).
ASK YOUR DOCTOR – Make sure to ask if there are cost-saving alternatives to the prescription they are providing. Many times, there are generic or different manufacturers that will save you money at the pharmacy.
PRESCRIPTION SUMMARY
Below is a high-level overview of your plan options and in-network benefit information:
You can view more details of these plans by accessing the medical benefit summaries provided under the Medical & Prescription section above.
RX Summary
A virtual visit lets you see and talk to a doctor from your mobile device or computer. When you use one of the provider groups in our virtual visit network, you have benefit coverage for certain non-emergency medical conditions.
WHEN CAN I USE A VIRTUAL VISIT?
When you have a non-emergency condition and:
- your doctor is not available;
- you become ill while traveling;
- When you are considering visiting a hospital emergency room for a non-emergency health condition.
*Your covered children may also use Virtual Visits when a parent or legal guardian is present for the visit.
Examples of Non-Emergency Conditions:
- Bladder infection
- Seasonal flu
- Sinus
- Sore throat
- Stomach
- Rash
- Bronchitis
- Diarrhea
- Fever
- Pink eye
HOW DOES IT WORK?
The first time you use a Virtual Visits provider, you will need to set up an account with that Virtual Visits provider group. You will need to complete the patient registration process to gather medical history, pharmacy preference, primary care physician contact information, and insurance information.
Each time you have a virtual visit, you will be asked some brief medical questions, including questions about your current medical concern. If appropriate, you will then be connected using secure live audio and video technology to a doctor licensed to deliver care in the state you are in at the time of your visit. You and the doctor will discuss your medical issue, and, if appropriate, the doctor may write a prescription* for you.
Virtual Visits doctors use e-prescribing to submit prescriptions to the pharmacy of your choice. Costs for the virtual visit and prescription drugs are based on, and payable under, your medical and pharmacy benefit. They are not covered as part of your Virtual Visits benefit.
*Prescription services may not be available in all states.
HOW DO I GET ACCESS?
Learn more about Virtual Visits and access direct links by downloading the Sydney Health App on your phone.
ANTHEM SERVICES
Interested in the services Anthem has available? This section will review the different services you have at your fingertips through Anthem.
- Sydney Health App
- Virtual Visits through the Sydney Health App
- 24/7 NurseLine
- Well-Being Coach
Did you know?
Anthem has a blog with Member News, Healthy Living, and Health Insurance basic articles. Click on the link below to review!

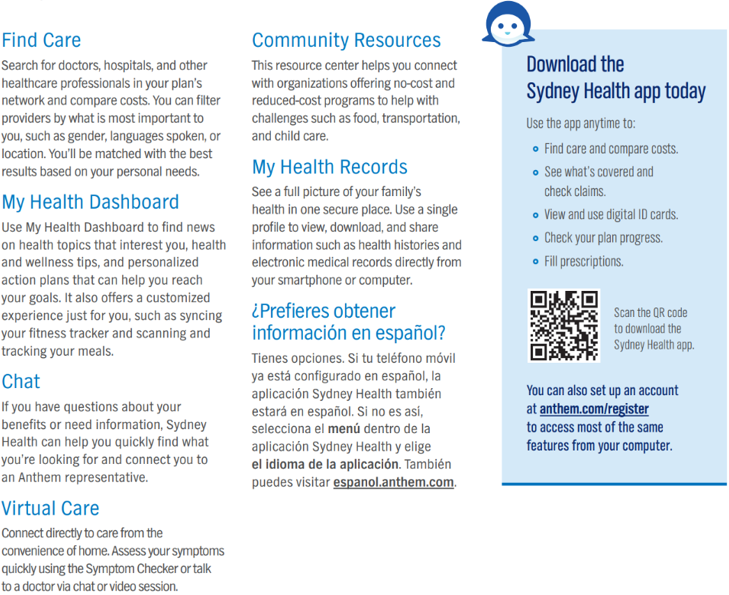
DOWNLOAD ANTHEM'S SYDNEY HEALTH APP
The SydneySM Health app is a free Anthem Blue Cross Blue Shield app that gives you fast and convenient access to your health insurance information right on your phone. It’s like having a personal health assistant in the palm of your hand.
What Can You Do With Anthem’s Sydney App?
Find A Doctor And Check Your Costs
Search for doctors, hospitals, labs, and other health professionals in your plan. You can search by name, location, and type of care. You can even filter by gender or languages spoken, and then check costs before you go to find what’s best for you.
View Your Claims
Check medical claims with one click. That means you can spend more time focused on your health and less on managing your healthcare benefits.
See All Your Health Coverage Benefits
The Sydney app shows you essential information at a glance. Whether that’s an overview of your plan, health reminders, or suggestions for wellness programs. You also can find your deductible, copay, and share of costs.
View And Use Your Anthem Digital ID Card
You’ll always have your most current Anthem ID card handy. You can use it just like a paper one when you visit the doctor, pay for care, and more.
Use The Chat To Find Answers To Your Questions
Just type your questions in the app and receive the answers you’re looking for. Plus, Anthem’s Sydney app can suggest resources to help you understand your benefits, improve your health, and save money.
HOW TO FIND IN-NETWORK PROVIDERS
The Find Care tool brings together details about doctors in your plan’s network. You can customize your search by name, location, specialty, or procedure. You also can compare information such as costs, languages spoken, and office hours.* To make sure a care provider is in your plan’s network, view the doctor or facility profile.
When you need care right away, the emergency room (ER) might be the first place that comes to your mind. However, the ER may not be the best choice in every situation. You have options when you have a sudden need for care, and knowing what they are can help you save time and money — and feel better sooner.
How to find the care you need - instructions for employees who are already enrolled:
- Go to www.anthem.com (click the link below) or download the Sydney Health App
- Then, log in to:
- Find a doctor if you don’t have a PCP.
- Have a virtual visit with a doctor using the Sydney Health App
- Find a retail health clinic, urgent care center, or ER.
- Choose the Find Care tab and follow the steps.
How to find the care you need - instructions for employees who are not currently enrolled in the medical:
- Go to www.anthem.com
- Network Blue Access PPO
- Click Basic search as a guest
- Select the type of plan or Network
- Choose Medical Plan or Network (may also include dental, vision or pharmacy benefits) from the drop-down
- Select Ohio
- Select Medical (Employer-Sponsored)
- Select Blue Access PPO and hit continue
- Select the type of plan or Network
- Enter your zip code and your physician's name
- or
- Search by Care Provider
24/7 NURSELINE
24/7 NurseLine serves as your first line of defense for unexpected health issues. You can call a trained, registered nurse to decide what to do about a fever, give you allergy relief tips, or advise you where to go for care. A nurse is always available to help answer your questions.
The Anthem Nurseline can help you with:
- finding care from a doctor, hospital, or specialist in your area.
- enroll you in health management programs through Anthem for certain health conditions.
- remind you about scheduling important screenings and exams.
- provide guidance during natural catastrophes and health outbreaks.
- offer links to health-related educational videos or audio topics.
Call the NurseLine today at (800) 337-4770.
What is the health management program?
Get tools and support for managing chronic conditions:
- diabetes
- asthma
- heart disease
Anthem health advocates can help you follow your healthcare plan.
For more information about the program, call Anthem at (866) 962-1071

ANTHEM ID CARD
Your Anthem Blue Cross Blue Shield insurance card contains all the necessary information you need to use your health insurance. Once you sign up for an Anthem plan, you will receive an Anthem ID card. The ID card envelope will not show that it is coming from Anthem. Be on the lookout for a blank white envelope in the mail.
DELTA DENTAL
Network: Delta Dental PPO
How do I find a Delta Dental In-Network Dentist?
- Click the link below or visit www.deltadentalid.com and select “Find a Dentist” wherever you are located or you may contact customer service at (208) 489-3580.
- You have the freedom to select the dentist of your choice; however, when you visit a participating in-network dentist, you will have lower out-of-pocket costs, no balance billing, and claims will be submitted by your dentist on your behalf.
Pre-treatment Estimate
- If your dental care is extensive and you want to plan ahead for the cost, you can ask your dentist to submit a pre-treatment estimate. While it is not a guarantee of payment, a pre-treatment estimate can help you predict your out-of-pocket costs.
Dental Health Education and Online Risk Assessment Tool
- Delta Dental provides an Oral Health and Wellness site that includes an interactive risk assessment tool that will assess your risk of dental disease. Any member can access a vast array of wellness topics, articles and the interactive risk assessment. Click the link below to learn more.
Looking for more details about how items are covered? Click on the link below to view the formal Benefit Summary

Below is a high-level overview of your plan option and in-network benefit information:
You can view more details of this plan by accessing the benefit summary provided below.
VISION
Directions Group offers vision coverage through Avesis to help pay for eye exams, prescription glasses and contact lenses. You receive a higher level of benefits when you see a provider in network, however, out-of-network coverage is provided but may only be handled as reimbursements in some situations. Please note: Members may choose between prescription glasses (lenses and frame) and contact lenses, not both.
Did You Know?
Eyes can give doctors a clear picture of overall wellness. That’s why vision care—and vision benefits—can help employees stay healthy. A comprehensive eye exam can detect early signs of serious health problems, such as:
- Diabetes
- Heart disease
- High blood pressure
- High cholesterol
- Glaucoma and cataracts
To find out if your provider is in-network, please visit the website below.
VISION SUMMARY
Below is a high-level overview of your plan options and in-network benefit information:
You can view more details of these plans by accessing the benefit summaries provided above.
Vision Benefit Summary
BASIC LIFE AND VOLUNTARY LIFE
Life insurance is an important part of your financial security. Life insurance helps protect your family from financial risk and sudden loss of income in the event of your death. Accidental Death & Dismemberment (AD&D) insurance is equal to your Life benefit in the event of your death being a result of an accident and may also pay benefits for certain injuries sustained.
Basic - Employer Paid 1X Salary up to $200,000
A sudden accident or death can leave you or your loved ones in a vulnerable position. Employees have the opportunity to enroll in Term Life and Accidental Death & Dismemberment insurance which will supplement lost income in the event of an accident or death. If you choose to enroll in employee coverage, this will be in addition to your employer-provided Basic Life coverage.
Voluntary - Employee Paid Life
Coverage is also available for your spouse and/or child dependents, but only after you've elected coverage for yourself. A sudden accident or death can leave you or your loved ones in a vulnerable position. Employees have the opportunity to enroll in Term Life and Accidental Death & Dismemberment insurance which will supplement lost income in the event of an accident or death. If you choose to enroll in employee coverage, this will be in addition to your employer-provided Basic Life coverage. Review the full benefit summary below for additional details.
Employee: $10,000 increments up to $500,00 (GI $100,000)
Spouse: $5,000 increments up to $500,00 (GI $25,000)
Children: $2,000 increments up to $10,000
The portability provision allows you to continue Voluntary Term Life Insurance upon loss of eligibility or termination of employment in these situations:
- Group policy discontinues the eligibility of a class of employees to which you belong
- You retire
- You are terminated or change jobs
This Policy will port into a Term policy.
You have 30 days from the loss of eligibility date to port your Voluntary Term Life.
Conversion allows you to convert your Voluntary Term Life Insurance to an individual life insurance policy in these situations:
- Employment ends
- You stop being a member of an eligible class of employees
- Dependent loss of eligibility
- The policy terminates
This policy will convert to a Permanent Whole Life policy.
You have 30 days from the loss of eligibility date to convert your Voluntary Term Life.
Beneficiary Designation
Who's Your Beneficiary?
Naming a beneficiary is a crucial part of electing life insurance. Also, don't forget to update your primary or secondary beneficiary if you experience a life event, such as a divorce or birth of a child.
Primary Beneficiary: Your primary beneficiary receives your benefits in the event of your death.
Contingent Beneficiary: Your contingent beneficiary receives your benefit, in the event that your primary beneficiary cannot.
*Please make sure your beneficiary information is up to date with your HR office*
*Guaranteed Issue (GI) and Evidence of Insurability (EOI)
When you are first eligible (at hire) for Voluntary Life and AD&D, you may purchase up to the Guaranteed Issue (GI) for yourself and your spouse without providing proof of good health (EOI).
Any amount elected over the GI will require EOI. If you elect optional life coverage and are required to complete an EOI, it is your responsibility to complete the EOI and send it to the provider (address will be listed on your form). In addition, your spouse will need to provide EOI to be eligible for coverage amounts over GI, or if coverage is requested at a later date.
LONG-TERM DISABILITY
Long Term Disability
Long Term Disability insurance can pay you a weekly benefit if you have a covered disability that keeps you from working. Long Term Disability insurance can replace part of your income while you recover.
LTD Benefit Features
- Benefit begins after a 90-day elimination period if remain disabled
- Benefit equal to 60% of pay – the benefit is taxable income
- Pre-existing condition limitations apply for the first 12 months
DISABILITY SUMMARY
Disability Summary
- Premium: The amount paid for insurance coverage deducted from your paycheck on a per-pay-period basis.
- Deductible: The amount you must pay out of pocket for covered services before your insurance plan starts to pay.
- Copayment (Copay): A fixed amount you pay for covered services at the time of service, usually for doctor visits or prescription drugs.
- Coinsurance: The percentage of costs you pay for covered services after you've met your deductible.
- Out-of-Pocket Maximum: The maximum amount you'll have to pay for covered services in a plan year, after which your insurance plan pays 100% of covered costs.
- Network: The group of doctors, hospitals, and other healthcare providers contracted with an insurance company to provide services at discounted rates to plan members.
- Preventive Care: Healthcare services aimed at preventing illness or detecting health conditions early when treatment is most effective, often covered at no cost under insurance plans.
- Benefit: The healthcare services or items covered by an insurance plan.
- Preauthorization: The process of obtaining approval from your insurance company before receiving certain medical services or treatments.
- In-Network: Healthcare providers or facilities that have contracted with your insurance company to provide services at lower costs to plan members.
- Exclusion: Specific healthcare services or conditions that are not covered by an insurance plan.
- Lifetime Maximum: The maximum amount of money that an insurance plan will pay for covered services over the entire life of the policy.
- Grace Period: A specified period after the premium due date during which coverage remains in force even though the premium has not been paid.
- Coordination of Benefits (COB): A process used when an individual is covered under more than one health insurance plan to determine which plan pays first and how much each plan will pay.
- Explanation of Benefits (EOB): A statement sent by the insurance company to the insured individual explaining what medical treatments and/or services were paid for on their behalf.
Why go to an In-network provider?
- Going to an in-network provider means choosing a healthcare professional or facility that has a contract with your health insurance plan. In-network providers have agreed to offer their services at negotiated rates, which are often lower than what you would pay for out-of-network care. By visiting an in-network provider, you can take advantage of your health insurance plan's benefits, which may include lower copayments, coinsurance, and reduced out-of-pocket expenses.
Why should I go for my annual well checkup?
- Annual well checkups are essential for maintaining good health and preventing potential health issues. These visits allow your doctor to assess your overall health, monitor any chronic conditions you might have, and detect early signs of potential health problems. Regular checkups help identify health concerns before they become serious, ensuring timely intervention and a better chance for successful treatment.
What is the difference between generic and brand name drugs?
- Generic drugs are identical or bioequivalent to brand-name drugs in terms of active ingredients, safety, strength, dosage form, and intended use. The main difference is that generic drugs are usually more affordable because they don't have the research and development costs associated with brand-name drugs. The U.S. Food and Drug Administration (FDA) ensures that generic drugs meet the same rigorous standards for quality, safety, and effectiveness as their brand-name counterparts.
How do discount cards work on RX?
- Prescription discount cards provide discounts on medications at participating pharmacies. These cards are often available for free or at a low cost and can be used by individuals without insurance or those with high copayments. When you present the discount card at the pharmacy, it reduces the price of the medication, potentially leading to significant cost savings.
What happens if I go out of network?
- If you go out of network for healthcare services, it means you're seeing a provider or using a facility that doesn't have a contract with your health insurance plan. Out-of-network care typically results in higher out-of-pocket costs, including higher copayments, coinsurance, and potentially higher deductibles. Some health insurance plans may not cover out-of-network care at all, except in emergencies.
What is a SBC (Summary of Benefits and Coverage)?
- A Summary of Benefits and Coverage (SBC) is a document provided by health insurance companies to help individuals understand their health plan's key features and coverage details. It provides a summary of the plan's benefits, costs, coverage limits, and examples of common medical scenarios to help individuals compare different health insurance options and make informed decisions.
What is an EOB (Explanation of Benefits)?
- An Explanation of Benefits (EOB) is a statement sent by the health insurance company to the policyholder after a healthcare claim has been processed. The EOB provides a detailed explanation of the services provided, the amount billed by the healthcare provider, the amount covered by the insurance, and any remaining balance that the insured may be responsible for paying.
What should I ask my doctor?
- When visiting your doctor, consider asking questions related to your health condition, treatment options, medications, potential side effects, and any lifestyle changes you should make. You can also inquire about preventive measures, recommended screenings, and follow-up care. Don't hesitate to ask for clarification if there's anything you don't understand.
What is preventive care?
- Preventive care refers to healthcare services aimed at preventing or detecting health issues before they become more severe or chronic. Examples of preventive care include vaccinations, screenings (e.g., mammograms, colonoscopies), regular checkups, counseling on healthy behaviors, and interventions to manage risk factors.
Where can I get my ID card?
- You can typically get your health insurance ID card from your insurance provider. Many insurers offer electronic versions of the ID card through their mobile apps or member portals. Alternatively, you can request a physical ID card to be mailed to you.
Who do I contact if I have a QLE (Qualifying Life Event)?
- If you experience a Qualifying Life Event (QLE), such as marriage, birth/adoption of a child, divorce, loss of other health coverage, or a change in household income, you should contact your employer's HR department or your health insurance provider promptly. They can guide you through the process of updating your health insurance coverage or enrolling in a new plan if necessary.