Plan Year 1/1/2023 - 12/31/2023
This Benefits Hub was designed to be an interactive, centralized resource for you and your dependents to visit both during open enrollment and throughout the year. Your Hub will serve as your go-to resource for benefits related questions. You’ll be able to access enrollment information, important benefit documents and different tools to help you understand your benefit offerings.
Open Enrollment: 11/18/2022 - 12/7/2022
The Benefit choices you make during your initial enrollment or annual open enrollment remain in effect for the entire year.
You can, however, modify your elections under certain circumstances, called "Qualifying Events". These are events such as marriage, divorce, birth or adoption of a child, loss of eligibility under another plan. If you experience a qualifying event, you must report the event to Human Resources within 30 days of the quailfying event.
QUALIFYING LIFE EVENTS
MEDICAL
NETWORK: BlueChoice PPO
How do I find an In-Network Provider?
Use the helpful link below! In-Network providers can also be found on your provider’s website at www.bcbstx.com under “Find Care”. Select "Find a Doctor or Hospital" and then you can search by provider/facility name or search by specialty.
Did You Know?
- Preventive Services are covered at 100% In-Network and copays & deductibles do not apply.
- You pay less out of pocket if you receive care from an In-Network provider.
- You do not need a referral to see a Specialist.
You have 2 medical plans to choose from. Compare the options in the chart below to see the changes to the plans effective 1/1/2023!
Both plans have out-of-network benefits but you will always save money by staying in network.
Summaries of Benefits and Coverage
Extras from BCBS
Video Preview
Video Preview
Video Preview
Video Preview
PHARMACY
Prescription drugs are a vital part of your health care coverage. If you have prescription drug coverage through Blue Cross and Blue Shield of Texas (BCBSTX), this information can help you and your doctor get the most from your prescription drug coverage. The Pharmacy Benefit Manager for BCBS is Prime Therapeutics. You can access more information about your pharmacy coverage by visiting www.myprime.com
A drug list is a list of drugs that are covered under your prescription drug benefit. How much you pay out of pocket is determined by whether your drug is on the list and at what coverage level, or tier. A generic drug is often at the lower tier. See if your drug is covered by reviewing your formulary drug list using the link below!
Express Scripts® Pharmacy, the mail order pharmacy for members with BCBSTX prescription drug coverage, provides safe, fast and cost-effective pharmacy services that can save you time and money. With this program, you can obtain up to a 90-day supply of long-term (or maintenance) medications through Express Scripts® Pharmacy.
Ordering Through Express Scripts® Pharmacy
Getting Started Online
You have more than one option to fill or refill a prescription online or from a mobile device:
- Visit express-scripts.com/rx . Follow the instructions to register and create a profile.
- Log in to myprime.com and follow the links to Express Scripts® Pharmacy.
Order Over the Phone
Call 1-833-715-0942, 24/7, to refill, transfer a current prescription or get started with home delivery. Please have your member ID card, prescription information and your doctor’s contact information available.
Video Preview
DEDUCTIBLE DOES NOT APPLY TO PHARMACY BENEFITS.
Review your prescription copays for each plan in the chart below!
HEALTH REIMBURSEMENT ARRANGEMENT (HRA) ADMINISTERED BY WEX
A Health Reimbursement Arrangement (HRA) is a benefit provided by your employer that sets money aside for you to spend on eligible healthcare expenses.
NEW! The HRA will reimburse up to $1,500 of all Section 213d eligible expenses (the same as the FSA). The HRA will be tied to your WEX debit card and, if you have an FSA, the HRA will pay first. Keep this in mind when considering how much you want to contribute to your FSA.
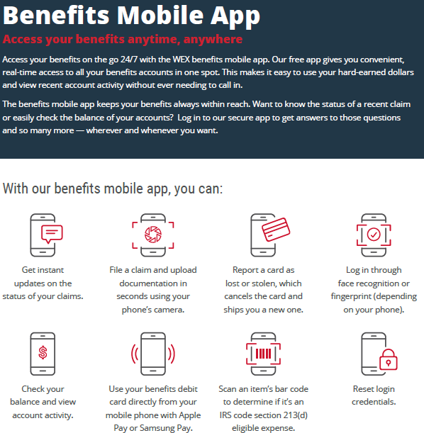
You can download the mobile app at on Google Play and the Apple Store.
FLEXIBLE SPENDING ACCOUNT (FSA) ADMINISTERED BY WEX
HEALTH CARE FSA
MAXIMUM ANNUAL CONTRIBUTION | $3,050
All eligible health care expenses – such as deductibles, medical and prescription copays, dental expenses, and vision expenses – can be reimbursed from your general purpose FSA account.
HERE’S HOW IT WORKS
An employee earning $30,000 elects to place $1,000 into a Health Care FSA. The payroll deduction is $110.42 based on a 24 pay period schedule. As a result, the insurance premiums and health care expenses are paid with tax-free dollars, giving the employee a tax savings of $574.
DEPENDENT CARE FSA
The Dependent Care FSA allows you to pay for eligible dependent care expenses with tax-free dollars so that you and your spouse can work or attend school FT.
Unlike the Health Care FSA, funds in a Dependent Care FSA are only available once they have been deposited into your account and you cannot use the funds ahead of time.
- You may set aside up to $5,000 annually in pre-tax dollars, or $2,500 if you are married and file taxes separately from your spouse.
- If you participate in a Dependent Care FSA, you cannot apply the same expenses for a dependent care tax credit when you file your income taxes.
IMPORTANT: PAYING FOR ELIGIBLE SERVICES & EXPENSES
Visit the FSA Store at www.FSAstore.com, where you can purchase FSA-eligible products without a prescription online.
Although you do not need to file for reimbursement when using your FSA debit card, you may be required to submit documentation, so be sure to save your receipts.
If you use a personal form of payment to pay for eligible expenses out-of-pocket, you can submit an FSA claim form along with your original receipts for reimbursement.
A full list of qualified expenses can be found in IRS Publication 502 at www.irs.gov.
DENTAL
(Same carrier, enriched benefits!)
You may select the dentist of your choice. However when you visit a participating in-network dentist, you will have lower out- of-pocket costs, no balance billing, and claims will be submitted by your dentist on your behalf. When you receive care from an out of network provider, benefits will be based on the 90th percentile of usual and customary charges.
PRE-TREATMENT ESTIMATE
If your dental care is extensive and you want to plan ahead for the cost, you can ask your dentist to submit a pre-treatment estimate. While it is not a guarantee of payment, a pre-treatment estimate can help you predict your out-of-pocket costs.
How do I find an In-Network Provider?
This dental plan offers deeper discounts when you visit a provider that is In-Network. In-Network providers can be found by selecting the link below. Choose "Search for a dentist" and then enter your zip code.
VISION
(Same carrier, enriched benefits!)
DID YOU KNOW?
- Eye exams can help detect serious eye and general health conditions sooner: high blood pressure, diabetes, heart disease, high cholesterol
- Babies should receive their first professional eye exam at 6 months
- 80% of learning in the first 12 years comes through the eyes
Under this plan, you may use the eye care professional of your choice. However, when you visit a participating in-network provider, you receive higher levels of coverage. If you choose to receive services from an out-of-network provider, you will be required to pay that provider at the time of service and submit a claim form for reimbursement. Your Principal plan uses the VSP network.
To find out if your provider is in-network, please visit the link below or you may call member services at 800-877-7195.
LIFE AND AD&D
Group Life
Life insurance is an important part of your financial security as it helps protect your family from financial risk and sudden loss of income in the event of your death. AD&D (Accidental Death & Dismemberment) insurance is equal to your Life benefit in the event of your death being a result of an accident, and may pay benefits for particular injuries sustained.
Basic Life / AD&D insurance is a company paid benefit, provided to you at no cost. Coverage is with Principal and will be 1 x salary up to $50,000. Keep in mind, your life insurance will reduce by 35% of the original amount at age 65 and 15% at age 70.
Supplemental Life
In addition to your employer provided Basic Life insurance coverage, you have the opportunity to enroll in voluntary/optional/supplemental Life insurance coverage.
Coverage is also available for your spouse and/or child dependents, however, It is required that you elect coverage for yourself in order to elect coverage for your dependents. See summary for details.
*Guaranteed Issue (GI) and Evidence of Insurability (EOI)
When you are first eligible (at hire) for Voluntary Life and AD&D, you may purchase up to the Guaranteed Issue (GI) for yourself and your spouse without providing proof of good health (EOI).
Any amount elected over the GI will require EOI. If you elect optional life coverage and are required to complete an EOI, it is your responsibility to complete the EOI and send to the provider (address will be listed on your form). In addition, your spouse will need to provide EOI to be eligible for coverage amounts over GI, or if coverage is requested at a later date.
BENEFICIARY
It’s very important to designate beneficiaries. Taking a few minutes to designate your beneficiaries now will help ensure that your assets will be distributed according to your direction.
AT OPEN ENROLLMENT:
•If you are currently enrolled, you may choose to increase your current Supplemental Life coverage by adding an additional $10,000 or $20,000 in coverage for yourself with no EOI required (up to the GI amount). Every year during open enrollment, you can continue to increase your coverage up to the maximum benefit. If you have coverage for yourself, you can also add or increase coverage for your spouse and children with no health questions asked.
•For example: Employee currently has $30k, they could increase to $40k or $50k at open enrollment without EOI.
•Any employee who previously declined Supplement Life coverage and wants to add the coverage at Open Enrollment can purchase $10,000 or $20,000 in coverage for themselves with no health questions and Spouses can add $5,000 or $10,000 (up to the GI amount). (Spouse amt may not exceed Employee amt)
DISABILITY
Short-Term Disability (Same carrier, enriched benefits!)
Everyday illnesses or injuries can interfere with your ability to work. Even a few weeks away from work can make it difficult to manage household costs.
This employer paid Short Term Disability coverage provides financial protection for you by paying a portion of your income, so you can focus on getting better and worry less about keeping up with your bills.
Elimination Period - Benefits begin after 1st day of disability due to injury or 8th day for disability due to illness
Benefit Duration - Payments may last up to 13 weeks (You must be sick or disabled for the duration of the waiting period before you can recieve a benefit payment.)
Coverage Amount - Covers 60% of your weekly income, up to a maximum benefit of $1,500 per week.
Pre-existing Condition - Does not apply if you haven’t been seen by a doctor or prescribed medication for an injury or sickness in the last 6 months or if your disability happens after 24 consecutive months of coverage. If you had symptoms during the preceding 6 months that would cause a reasonable person to seek a diagnosis, care or treatment, that may be pre-existing condition.
Long-Term Disability (Same carrier, enriched benefits!)
Serious illnesses or accidents can interrupt your life, and your ability to work for months – even years. Long Term Disability is provided to full time eligible employees at no cost to you.
Elimination Period - Benefits begin after 90 days
Benefit Duration - Varies based on your age when you become disabled (see summary for more details)
Coverage Amount - Covers 60% of your monthly income, up to a maximum benefit of $6,000 per month.
Pre-existing Condition - Does not apply if you haven’t been seen by a doctor or prescribed medication for an injury or sickness in the last 6 months or if your disability happens after 12 consecutive months of coverage. If you had symptoms during the preceding 6 months that would cause a reasonable person to seek a diagnosis, care or treatment, that may be pre-existing condition.