Table of Content
- Header
-
Page
- Welcome!
- Guides
- Benefits Eligibility / How to Enroll
- Eligibility
- New Hire
- Qualifying Life Event
- Enrollment
- Medical Benefits
- Medical Benefits
- Medical Plans
- Compare Plans
- Health Plan
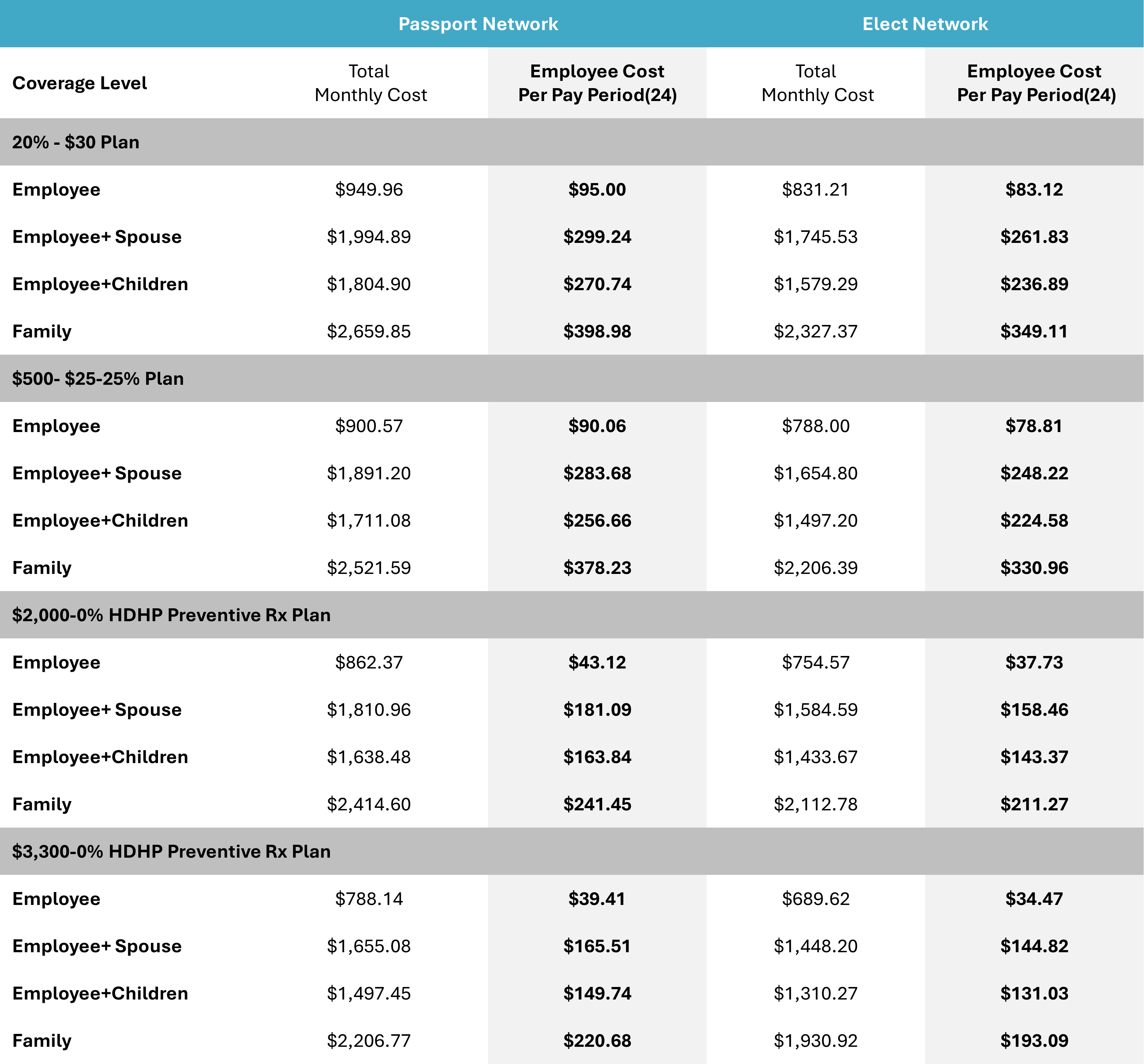
- Health Rates
- Medica Value Added Service
- HSA / FSA
- HSA intro
- Understanding Your HSA
- Eligiability
- Health Savings Account (HSA)
- FSA
- New Sub Section
- Understanding Your FSA
- Questions
- Flexible Spending Accounts (FSA)
- Commuter Account
- Commuter Account Eligiability
- Metro Transit
- Commuter Accounts
- Dental
- Dental
- Dental Plan and Rates
- Dental Prevention First
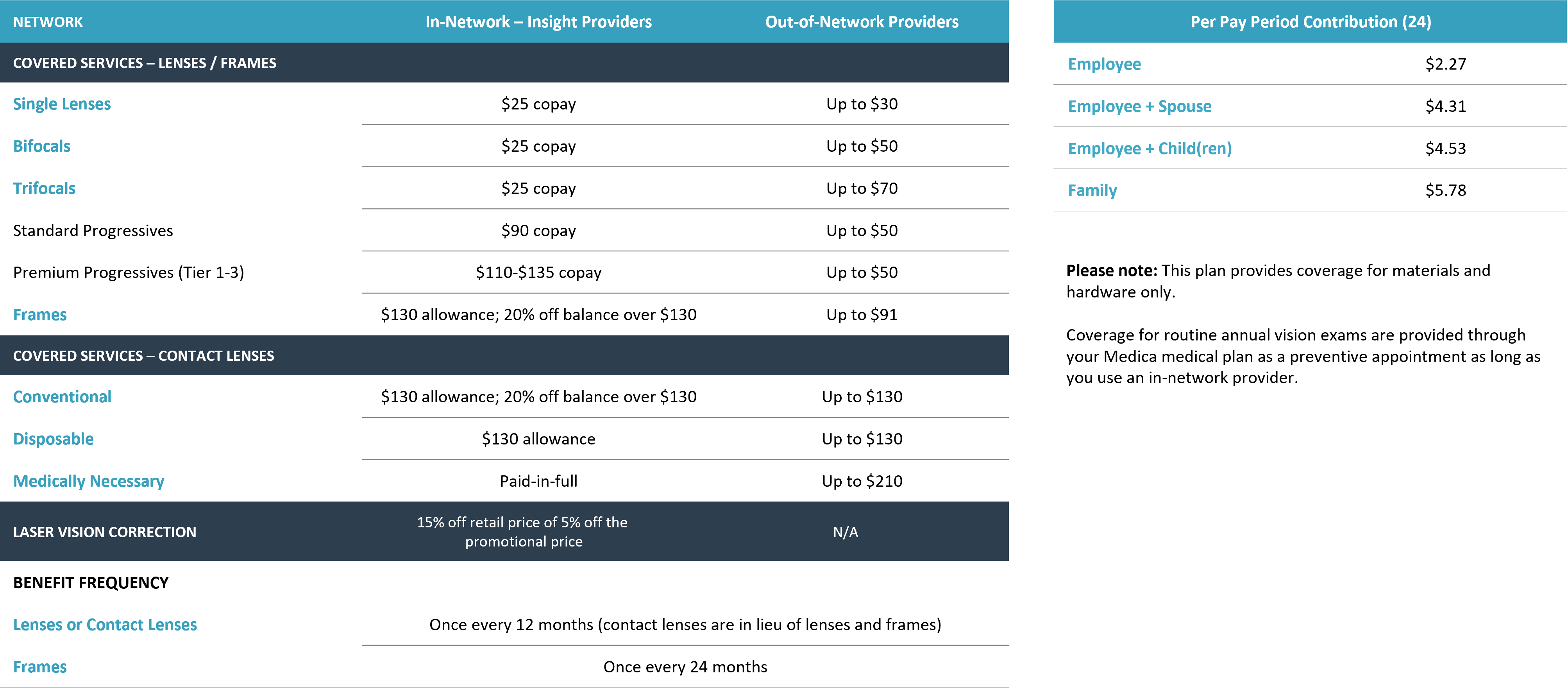
- Vision
- Vision
- Vision Plans and Rates
- Vision Benefits Fair
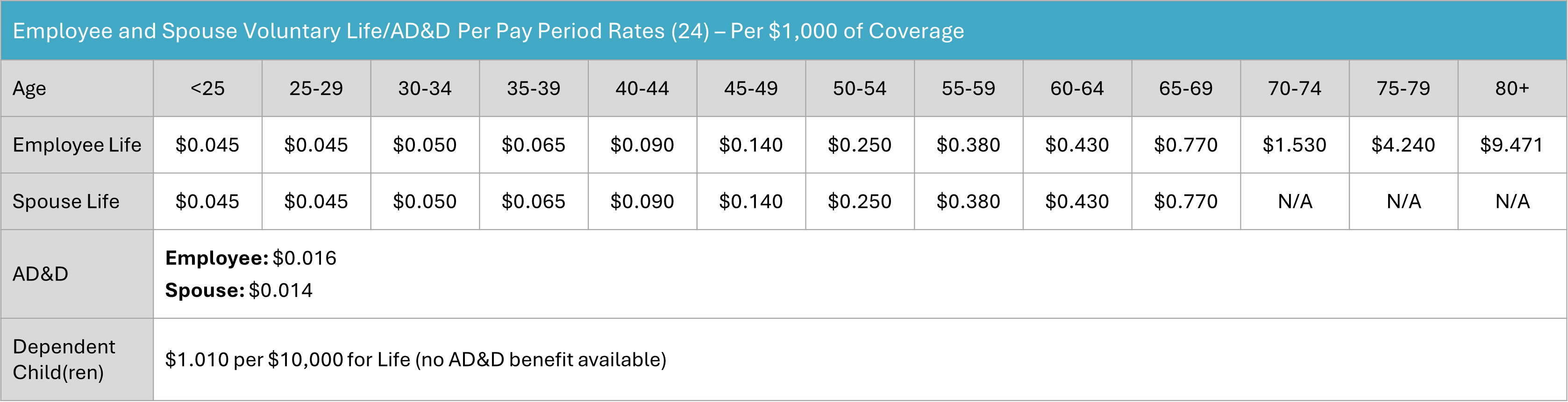
- Life & Disability
- Life and AD&D Insurance
- Age Rates
- What Will My Beneficiary Receive?
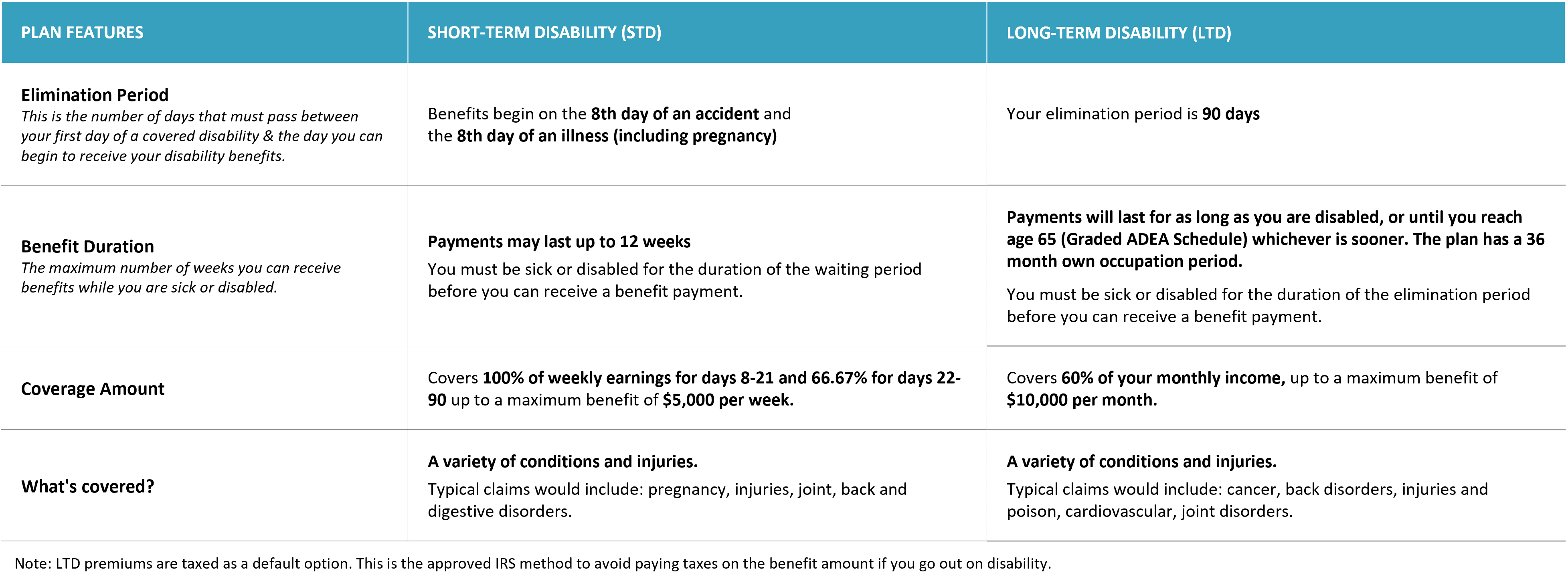
- Disability Benefits (STD/LTD)
- Disability Insurance
- Travel AD&D Insurance
- Worksite Benefits
- Worksite Benefits 2
- Sun Life Value Adds
- Additional Benefits
- Pet Insurance
- Pet Insurance 2
- Legal & ID Theft
- 401(k)
- 401k 2
- New Sub Section
- Paid Time Off & Holidays
- Elective Programs
- Contact Us
- Picture / Video Assets
- Misc.
- Footer
TPT- Twin Cities PBS believes that every employee plays an important role in our company’s success and that is why we strive to provide you with a benefits program that rewards you for the hard work and dedication you put forth everyday.
We genuinely care about your health and the well-being of your family. That's why TPT is proud to offer an extensive range of benefits that have been carefully crafted to prioritize your overall health and financial security. These benefits offer employees the option to pick quality medical care, dental care, life insurance, and other related services.
This benefits guide is aimed to help you understand the benefit options available to you and your eligible dependents, answer questions you may have so that you can make an informed selection of the benefits that best fit your needs. The information provided here can be used as a reference throughout the year.
Our benefit program undergoes an annual review to ensure that it delivers the best possible combination of coverage, network access, and affordability for you and your family.
Please review the benefit guide and should you have any questions after reviewing the information provided here and/or in the benefits guide, please feel free to reach out to Human Resources.
Thank you!
Employee Eligibility
If you are an employee, regularly scheduled to work 20 or more hours per week, you are eligible for the benefits listed in this benefit guide. The only exception is the medical plan, you must work 30 or more hours per week to be eligible.
Dependent Eligibility
When you enroll yourself in the Benefit Program, you may also cover your eligible dependents for medical, dental, vision, optional life, worksite policies and Legal and ID Shield policies. Eligible dependents include:
Your legal spouse. This does not include a common law spouse or an ex-spouse.
Your (or your spouse’s) biological child, step child, legally adopted child, foster child, a child for whom legal guardianship has been awarded, and who are less than 26 years of age.
Unmarried dependent child who is physically or mentally disabled and is dependent on you for at least 50% of his or her support and maintenance, provided the child’s disability begins and the child is enrolled in the plan before the date the child reaches the age which coverage would otherwise end. Proof of disability is required.
The term ‘child’ refers to any of the following:
- A natural (biological) child;
- A stepchild;
- A legally adopted child;
- A child for whom legal guardianship has been awarded to the covered employee or the covered employee’s spouse; or
- Disabled dependents may be eligible if requirements set by the plan are met.

When to Enroll
New employees are eligible for benefits first of the month following 30 days of continuous, full-time employment. The only exception is the commuter benefit (parking/transit), you are eligible for this benefit on the date of hire.
If you do not enroll during the initial eligibility period, the next time you are able to enroll is during the annual open enrollment, unless you have a qualifying life event.
Qualifying Life Events
If you have a Qualifying Life Event and want to request a mid-year change, you must notify Human Resources and complete your election changes within 30 days following the event.
Be prepared to provide documentation to support the Qualifying Life Event. Common life events include; Marriage, Divorce, Birth, Loss/gain of available coverage by you or any of your dependents. A full list of qualifying events can be found in the ‘Required Notices’ packet.

IMPORTANT You cannot make changes to these elections during the year unless you experience a qualified family status change, which must be reported to Human Resources within 30 days of the event. If you separate from employment, COBRA continuation of coverage may be available as applicable by law. COBRA Continuation details can be found in the notices guide.

How to Enroll
Enrollment will be done on the UKG/UltiPro portal. Visit "Life Events" to enroll and/or make changes. During your enrollment period, it is necessary to carefully consider and choose your benefits, as they will remain in effect for one year.
Each year you will have the opportunity to modify your benefits package during the open enrollment period. With the exception of certain qualifying events, open enrollment is the only time benefit changes may be made. Should you have any questions please reach out to Human Resources.
Medical Insurance
Administered by Medica
Discover more about your coverage and plan choices here to ensure you find the perfect fit for you and your loved ones.
When choosing a health care provider, there’s a lot to consider. Is the doctor you want in your plan network? How about specialists? Are in-network hospitals and clinics close by? Learn more about the Healthcare options available to you.

Network Options
With each Medica plan, you have the freedom to choose between two networks. You choose which network you would like to participate in at open enrollment. Then, you decide whether to use in-network or out-of-network providers at the time of service. It is in your best interest to seek providers who are in-network this ensures you will receive the highest level of benefits at discounted costs.
Medica Choice Passport Network
This is Medica’s largest, national network. You have access to more than 1 million providers and more than 5,900 hospitals across the U.S. For care received within the Medica service area, you have the Medica Choice Passport open access network. For care received outside of the Medica service area (students, while traveling, etc.) you have access to the UnitedHealthcare national network. You are free to see any provider in the Medica network – without a referral – and you are not required to select a primary care clinic. The Mayo Clinic Health System is included as part of this network.
Medica Elect
This smaller network of providers have agreed to provide services at lower rates. With the Elect network, you will need to choose a primary care clinic/care system to be your medical home. All of your care will be coordinated by your primary care clinic, including referrals outside of the care system, if necessary. These networks will save you money on monthly premium costs. For care received outside of the Medica service area (students, while traveling, etc.) you have access to the UnitedHealthcare national network.
Twin Cities PBS offers four medical options providing coverage for preventive care, doctor’s visits, hospitalization, prescription drugs and more.
Copay Plans
Plan 1 | 20% - $30
Plan 2 | $500 - $25 - 25%
This plan requires that you pay a copay for office visits and prescription drugs. Preventive care is covered at 100%. All other covered services, including hospitalization, ER, imaging and x-rays associated with an office visit, etc., are subject to deductible and/or coinsurance. Once you’ve met the annual out-of-pocket maximum, the plan pays 100% of covered services for the rest of the plan year as long as services are in-network.
High Deductible Health Plan with Preventive Rx
Plan 3 | $2,000 - 0% HDHP Preventive Rx
Plan 4 | $3,300 - 0% HDHP Preventive Rx
The High Deductible Health Plan (HDHP) requires that you meet an annual deductible before the plan will start to pay for covered services – with the exception of preventive care, which is covered at 100% with no deductible. Once you have met the deductible, you and the plan share the cost of services – called coinsurance – until you meet the out-of-pocket maximum. At that time, the plan will pay 100% of the cost of eligible services for the remainder of the calendar year. Twin Cities PBS makes an HSA contribution for employees that enroll in the HDHP plan to help offset deductible and out-of-pocket expenses.
How to find a Primary Care Clinic (PCC)
- Go to tpt.welcometomedica.com/home
- Choose “Find care” and then Medica Elect network
- Under providers + facilities click on Find a provider or facility
- Set your location area in the upper right corner, then select either “Facilities by name” or “Facilities by Type” tile
- Select the search spyglass icon but do not enter anything in the search bar
- From the results, select “Filters” and check “Yes” in the “Eligible Primary Care Clinic (PCC) section. Each provider result will include the 11-digit PCC number and care system affiliation
To find a Network provider, or learn more about your plan options
Go to tpt.welcometomedica.com/home or for assistance by phone, call Medica customer service at 800.952.3455
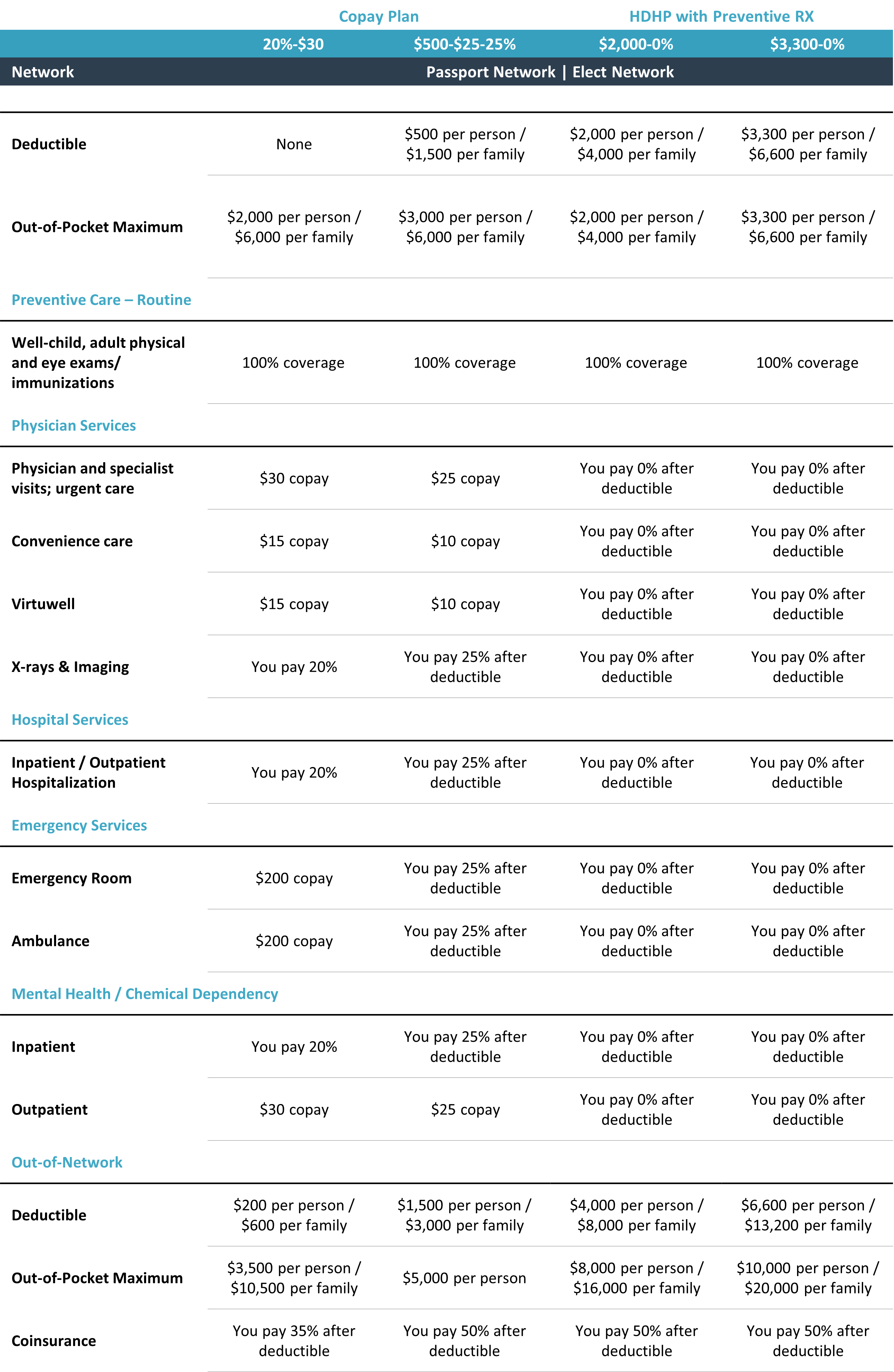
Compare Plans
Learn about your plans to see the differences between benefits and premiums paid, so you can confidently choose the plan that suits you best.
Medica Value Added Benefits
Medica responds to your needs with tailor-made services and resources that support you in improving your health and making the most of your benefits., Best of all, these are all a part of your benefit plan once you become a member. We’re ready when you are. Call Customer Service for any of the resources listed below.
Employee Assistance Program
When you need help with life’s challenges. Sometimes life throws you a curveball. Whether it’s financial troubles, personal issues or family problems, we can help. Just call 800-626-7944 any time of day or night, any day of the year to talk with a counselor. They’ll help you find the resources you need to get back on track.
Click here to learn more Medica | Employee Assistance Program Information for Members
Health Rewards Program
Get inspired to make positive changes. Taking steps to improve your health might be easier than you think. Whether you want to stress less, quit smoking or eat more fruits and veggies, My Health Rewards by Medica® makes it fun – and rewarding. You’ll earn gift cards as you complete activities personalized just for you.
To find your own path to better health, log on to mymedica.com and choose the Health & Wellness tab.
AbleTo - Behavioral Health Support
Access self-care techniques, coping tools, meditations, sleep tracking, and more at no additional cost - anytime, anywhere with Self Care by AbleTo. Check-in, track your progress, and explore personalized content that you can move through at your own pace on your mobile device. Build skills you can use for life to feel better.
To get started, visit Virtual Behavioral Health Care and select "Medica" when asked for your access code. After you register, download the AbleTo app.
24-Hour Health Support
Trusted answers any time of day or night. Worried that your stomach bug could be serious? Wondering what to do about that cough that won’t go away? The advisors and nurses at Medica CallLink® can help. They’re available 24 hours a day, 365 days a year to answer your questions and help you make smart decisions about your health. Just call 800-962-9497 (TTY users, call 711).
Click here to learn more Medica | CallLink Nurse Line Information for Members
Omada
Empowers you to build healthy behaviors that last. Omada is a digital lifestyle change program for people at risk for chronic conditions like prediabetes, hypertension, high cholesterol and cardiovascular disease. Participants learn how to make meaningful changes and sustain those behaviors.
Click here to learn more Healthy is for everyone | Omada Health
Ovia Health
Step into personalized guidance, support and coaching for your entire parenthood journey with the Ovia Health apps. They give you on-demand support and clinically backed guidance to help you achieve your health goals, whether that's tracking your period, getting pregnant, or navigating pregnancy, postpartum and parental wellness. Available to women ages 18-46.
Click here to learn more Individuals - Ovia Health
Learn all about your HSA and FSA to maximize your
healthcare savings potential!

Health Savings Account (HSA)
Administered by Optum Bank
Take charge of your health care spending with a Health Savings Account (HSA).
Contributions to an HSA are tax-free, and no matter what, the money in the account is yours!
Enrolled in an HSA Eligible Health Plan?
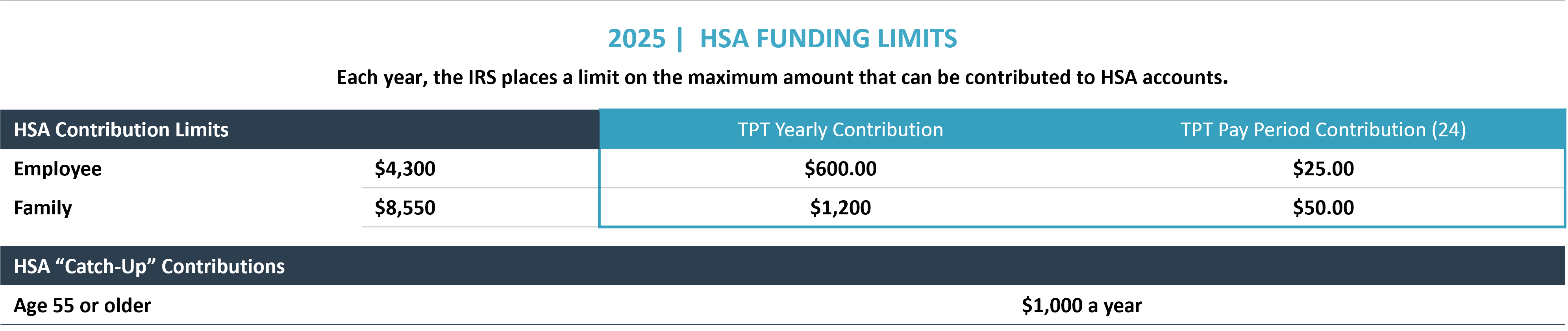
If you enroll in the $2,000-0% or $3,300-0% HDHP Preventive Rx Plans, you can contribute to a Health Savings Account (HSA). An HSA is a tax-free savings account is owned by you, is 100% vested from day one, and let’s you build up savings for future needs.
The funds may be used to pay for qualifying healthcare expenses not covered by insurance or any other plan for yourself, your spouse, or tax dependents. You decide how much you would like to contribute, when and how to spend the money on eligible expenses, and how to invest the balance.
Understanding Your HSA
- Pre-tax contributions are deducted through payroll and deposited into your HSA account;
- You can use your HSA available funds to pay for qualified medical expenses tax-free;
- HSA funds can be used for non-eligible expenses but will be subject to regular income taxes and a 20% excise tax penalty.
- Unused funds remain in your account for future use and roll over each calendar year;
- HSAs remain with you even if you change health plans or companies. If you open an HSA and later become ineligible to make contributions, you can still use your remaining funds; and
- You can change your HSA contribution at any time during the plan year for any reason.
HSA Frequently Asked Questions
When are funds available?
The funds are available upon deposit from your paychecks. You do not have access to the money until it is in your account. You can use funds for eligible expenses now, or when you retire.
How do I set-up my online account?
After your first payroll deductions for your benefits, go to OptumBank.com and complete the set-up of your account.
When will I get my card?
You will get your card within 30 days of your eligibility date.
How can I access my funds?
Using your debit card or completing documentation within your online account.
When do I get statements for my account, are they mailed or sent electronically?
You will get quarterly statements for the activity of your account. You can elect after setting up your account to get these in your email mail, rather than having them mailed to your home address.
At what point can I start investing my funds?
When you have at least $2000 in your account, you can make elections for your money to be invested at Optumbank.com
Who do I call if I have questions about the status of my account or debit card?
Optum Customer Service 1-844-326-7967
HSA Eligibility Requirements
To have an HSA and make contributions to the account, you must meet several basic qualifications:
- To be eligible to open and contribute to an HSA, you must have coverage under a qualified High Deductible Health Plan (HDHP).
- Participants cannot be covered by any other health insurance plan (this exclusion does not apply to certain other types of insurance, such as dental, vision, disability or long-term care coverage);
- Participants cannot participate in a Healthcare FSA or spouse/domestic partner’s Healthcare FSA or Health Reimbursement Account (HRA).
- Participants cannot be enrolled in Medicare or Medicaid.
- You cannot be eligible to be claimed as a dependent on someone else’s tax return.
- You have not received Department of Veterans Affairs Medical benefits in the past 90 days, unless the Veteran has a disability rating. (There may be additional special circumstances, check with your tax preparer).
Please note: Between your employee contribution and employer contribution, you may not exceed the IRS maximum contribution limits.
Tax advantage
- Pay no taxes on the money you contribute
- Pay no taxes on interest you earn
- Pay no taxes when you withdraw money Triple-tax savings for you!
Eligible expenses
Eligible healthcare expenses for you and your enrolled dependents now or in the future (retirement). Visit www.IRS.gov and review Publication 502 for a list of eligible expenses
How to use the account
Use your HSA Card or pay out-of-pocket and submit your claim for reimbursement. Visit Health savings accounts (HSAs) (optumbank.com). Keep all receipts.
Funds roll over year to year
YES. The money in the account belongs to you, even if you leave TPT-Twin Cities PBS.
Flexible Spending Account (FSA)
Administered by WEX Health
Can be a great way to save money on taxes and pay for unexpected medical expenses.

Medical Flexible Spending Account
Maximum Annual Contribution | $3,300
The Medical Flexible Spending Account gives participants in the 20%-$30 and $500-$25-25% plans the opportunity to set aside pre-tax dollars to pay for qualified medical, dental and vision expenses. Examples of eligible expenses include deductibles and co-pays, prescription drug costs, over-the-counter medicines (if prescribed by a doctor), and other non-covered medical, dental, vision and hearing care expenses.
Limited Purpose Flexible Spending Account
Maximum Annual Contribution | $3,300
Participants in the $2,000-0% or $3,300-0% HDHP Preventive Rx Plans can contribute to a Limited Purpose Flexible Spending Account for Dental and Vision expenses ONLY.
Eligible Expenses
A full list of qualified FSA expenses can be found in IRS Publication 502 at www.irs.gov. You can learn more about FSA qualified expenses and also make purchases by visiting the FSA Store at fsastore.com.
Dependent Care FSA
Maximum Annual Contribution | $5,000
The Dependent Care FSA allows you to pay for eligible dependent care expenses with tax-free dollars so that you and your spouse can work or attend school full time. Unlike the Health Care FSA, funds in a Dependent Care FSA are only available once they have been deposited into your account – much like a checking account.
You may set aside up to $5,000 annually in pre-tax dollars, or $2,500 if you are married and file taxes separate from your spouse. If you participate in a Dependent Care FSA, you cannot apply the same expenses for a dependent care tax credit when you file your income taxes.
Medical FSA Rollover
Your medical FSA has a $660 (projected) roll over feature, which allows any amount of $660 or less remaining in your account at the end of the plan year to roll over into the new plan year. The first rollover will occur after the runout period ends on February 28, 2025.
“Use It” OR “Lose It”
If you don’t use the funds in your account by December 31, 2025, you’ll lose them. Estimate expenses carefully as a federal “use-it or lose-it” law applies for any amount remaining in your account at the end of the year – except for $660 which can be rolled over.
____
Eligible Dependent Care
Expenses Include:
‘Care’ for your dependent child who is under the age of 13 that you can claim as a dependent on your federal tax return;
‘Care’ for your dependent child who resides with you and who is physically or mentally incapable of caring for themselves; or
‘Care’ for your spouse, parent or grandparent who is physically or mentally incapable of caring for themselves and spends at least eight hours a day in your home.
‘Care’ is defined as: In-home baby-sitting services (not by an individual you claim as a dependent); care of a preschool child by a licensed nursery or day care provider; before and after-school care; summer day camp (provided it is not overnight); and in-home dependent day care.
Questions?
Click on the links below for more information or if you have additional questions about enrolling in a flexible spending account (FSA), or questions about an existing account, please contact participant services.
New to WEX and have questions about enrollment? Phone us at 844-561-1337
Current WEX participant and have questions? Phone us at 866-451-3399

Commuter Accounts
Administered by WEX Health
Commuter benefits allow you to put money from your paycheck aside each month, before taxes are taken out, for qualified mass transit and parking expenses.
Eligibility
You are eligible to participate in the Twin Cities PBS commuter benefit program on your date of hire if you are an active full-time employee. Please note that this is the only benefit that has a date of hire start date.
How the Plan Works
You may choose to enroll in either or both the parking and/or transportation element of the commuter accounts. You would be eligible to enroll in both the parking and mass transit benefit in a circumstance where you drive your car to a mass transit station to park in order to commute the remainder of your travel to work by bus or train.
What Does It Cover?
Commuter funds can be used on a variety of transportation and parking expenses that allow you to travel to and from work. Eligible modes of transportation include but aren’t limited to: Train, Bus, Subway, Vanpool (must seat at least 6 adults), Parking or Parking meter near you or your place of employment.
Other Contract Parking Options
Employees who are interested in signing up for a monthly parking contract in the adjacent ramp or nearby surface lot may contact James Henjum in payroll.
IRS Regulations
The IRS sets the maximum dollar amount you can set aside each month as a part of your commuter benefit. The monthly pre-tax contribution limit is
Parking $325
Transit $325
Availability of funds
Your funds become available as you contribute to the plan, generally within 2-3 days after your payroll contribution.
Contribution changes
You can adjust the amount you contribute to the plan each month at any time. No qualifying event is needed.
Rollovers and use-or-lose
The commuter plan is flexible and your funds will continue to roll over month to month until the funds are used. However, your funds will no longer be available if you terminate employment.

Metro Transit
As an employee of Twin Cities PBS, you are eligible to purchase discounted Metro Transit Go-To Cards through payroll deduction. We purchase the stored value cards in $20 increments starting at $20 per month.
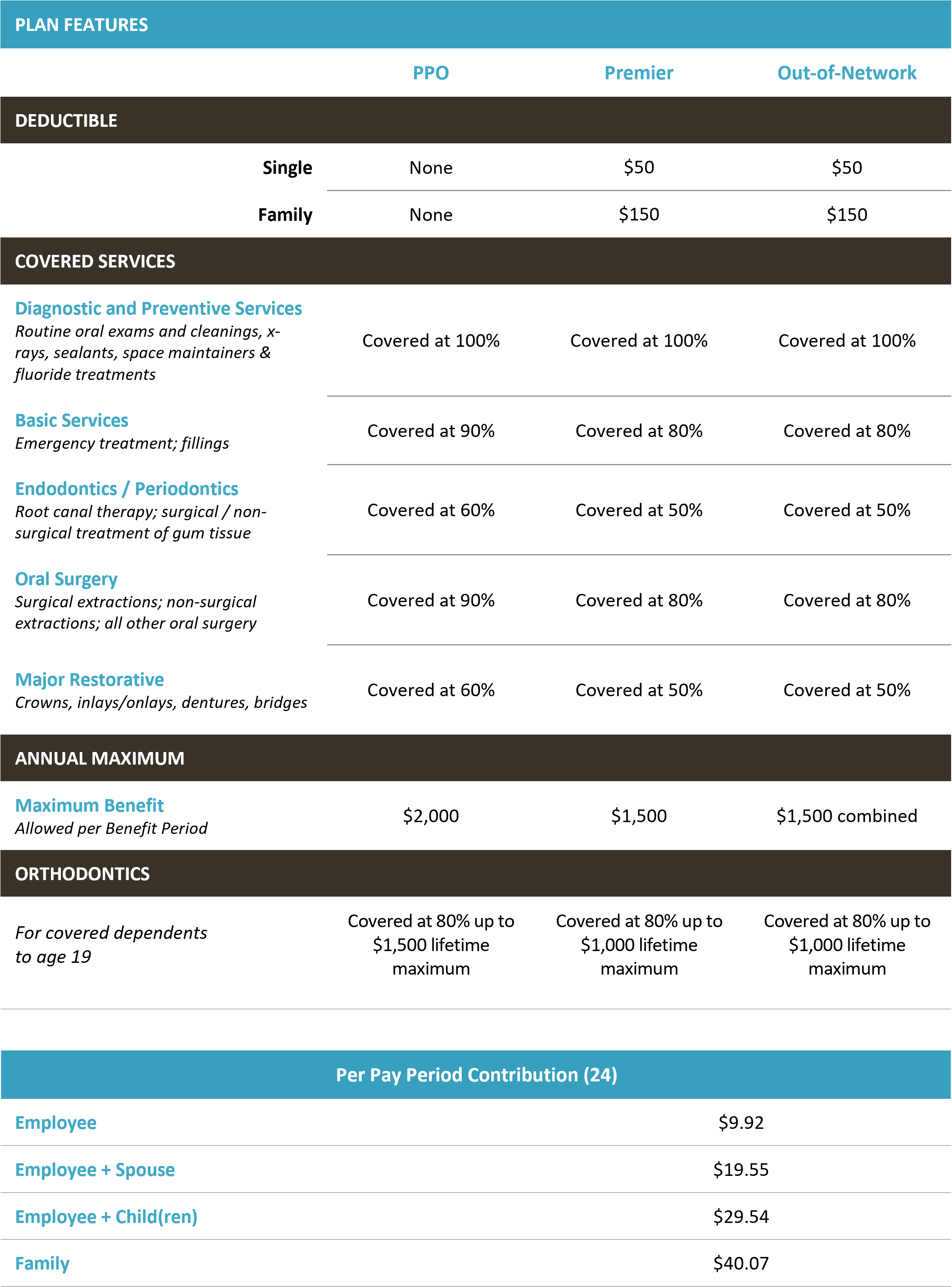
Dental Insurance
Administered by Delta Dental
Staying healthy includes good dental care. Twin Cities PBS’ dental plan provides the comprehensive coverage necessary to help you and your family maintain good dental health.

Plan participants have the flexibility to see any dentist they choose. However, greater discounts and benefits are available by seeing an in-network dentist. You will receive better discounts and the highest level of benefits if you choose a PPO dentist
Find a Provider by going to deltadentalmn.org and select the Delta Dental PPO or Delta Dental Premier Networks. Enter your zip code and the distance you are willing to travel to find a provider in your area.
Compare Network Plans
Compare plans side-by-side with to see the differences between benefits and premiums paid, so you can confidently choose the plan that suits you best.
Common Terms
Pre-Treatment Estimate
If your dental care is extensive and you want to plan ahead for the cost, you can ask your dentist to submit a pre-treatment estimate. While it is not a guarantee of payment, a pre-treatment estimate can help you predict your out-of-pocket costs.
Dual Coverage
You might have benefits from more than one dental plan, which is called dual coverage. In this situation, the total amount paid by both plans can’t exceed 100% of your dental expenses. And in some cases, depending on the specifics of the plans, your coverage may not total 100%.
Limitations and Exclusions
Dental plans are intended to cover part of your dental expenses, so coverage may not extend to your every dental need. A typical plan has limitations such as the number of times you can receive a cleaning each year. In addition, some procedures may be not be covered under your plan, which is referred to as an exclusion.
Prevention First!
Preventive care services are covered at 100%.
Your dental health is an important part of your overall health. Make sure you take advantage of your preventive dental visits.
How do I find an In-Network Provider?
To find in-network preferred providers, go to www.deltadentalmn.org and select the Delta Dental PPO or Delta Dental Premier Networks. Enter your zip code and the distance you are willing to travel to find a provider in your area. Or you can call 800.448.3815.

Vision Insurance
Administered by EyeMed
This coverage is a voluntary benefit that features coverage for prescription glasses, contact lenses, as well as other vision-related items.
Under this plan, you may use the eye care professional of your choice. However, when you visit an EyeMed in-network provider, you receive higher levels of coverage. If you choose to receive services from an out-of-network provider, you will be required to pay that provider at the time of service and submit a claim form for reimbursement.

Access Your Virtual Benefit Fair
See available benefits, find in-network providers near you and discover how to become an EyeMed member. You can also get answers to frequently asked questions. Access the Virtual Benefit Fair at your convenience through your computer, tablet or mobile device.
To get started, click the link below and enter in the password: KK814VJX
Basic Life And AD&D Insurance
Administered by Sun Life
You can’t always predict – or control – your life. But you can prepare for it.
Protecting the financial interests of your loved ones in the event of your death or serious injury can be invaluable.

Basic Life Insurance
Life and accident insurance are valuable benefits for you and your family. TPT-Twin Cities PBS automatically provides you with Basic Life and Accidental Death and Dismemberment (AD&D) insurance. Eligible employees automatically receive 2 times annual salary plus $20,000 of the employer-paid Life and AD&D benefit – there are no choices to be made. Any benefits paid out are tax-free to the recipient.
Voluntary Life and AD&D Insurance
You have the opportunity to purchase additional Life and AD&D insurance for yourself and your eligible dependents. To provide coverage for your dependents, you must first choose coverage for yourself. Also, keep in mind that your voluntary life selection should correspond with your voluntary AD&D selection.
Evidence of Insurability
New hires can elect coverage up to the guarantee issue amount without Evidence of Insurability (EOI). You must submit EOI within 30 days of your application when:
You enroll as a late entrant (enrolling outside of the new hire period)
When you apply for an increase in the benefit amount
When you apply for a benefit in excess of the Guarantee Issue (GI)

What Will My Beneficiary Receive?
In The Event That Death Occurs: Your Basic Life insurance is paid to your beneficiary. If death occurs from an accident: 100% of the AD&D benefit would be payable to your beneficiary(ies) in addition to your Basic Life insurance.

Disability Benefits (STD / LTD)
Administered by Sun Life
Disability coverage provides financial protection for you by paying a portion of your income, so you can focus on getting better and worry less about keeping up with your bills.
TPT-Twin Cities PBS provides full-time employees with short- and long-term disability income benefits– at no cost to you! Even a few weeks away from work can make it difficult to manage household costs.
In the event you become disabled from a non-work-related injury or illness, disability income benefits will provide a partial replacement of lost income. Please note that you are not eligible to receive disability income benefits if you are receiving workers’ compensation benefits.
Please note: To receive a benefit, your claim must be approved by SunLife.
Short-Term Disability (STD)
Everyday illnesses or injuries can interfere with your ability to work. Even a few weeks away from work can make it difficult to manage household costs.
Short Term Disability coverage provides financial protection for you by paying a portion of your income, so you can focus on getting better and worry less about keeping up with your bills.
Long-Term Disability (LTD)
Serious illnesses or accidents can come out of nowhere. They can interrupt your life, and your ability to work for months – even years.
Long Term Disability provides financial protection for you by paying a portion of your income, so you have financial support to manage your disability and your household.
Please note: LTD premiums are taxed as a default option. This is the approved IRS method to avoid paying taxes on the benefit amount if you go out on disability.
Travel AD&D Insurance
Twin Cities PBS provides additional coverage for business travel Accidental Death and Dismemberment (AD&D) insurance at no cost to the employee.
Eligibility and benefits are:
- Each active, full-time employee is covered with a principal sum of $75,000
- The policy covers losses while on a business trip, for Twin Cities PBS, from all accidents
- Business trip means travel authorized by Twin Cities PBS.
- Everyday travel to and from work is not included

Learn all about your worksite benefits including Accident, Critical Illness, and Hospital Indemnity and understand how they can support and enhance your health plan.
TPT-Twin Cities PBS provides eligible employees with the opportunity to participate in a variety of voluntary benefits. These voluntary benefits offered through SunLife are designed to help offset the cost of medical care, should you need it. If you would like to enroll in these benefits, please reach out to HR for enrollment forms.
Accident Insurance
Accident insurance can pay you money based on the injury and the treatment you receive, whether it’s a simple sprain or something more serious, like an injury from a car accident. The Accident Insurance Plan through SunLife includes off job coverage and can pay you a benefit for an emergency room treatment, stitches, crutches, injury-related surgery and a list of other accident-related expenses. The money is paid directly to you and you decide how to spend it. You can also purchase coverage for your spouse and dependent children.
Critical Illness
Critical Illness, including cancer, impacts so many lives. One of the greatest and most easily forgotten effects is the financial burden associated with such diagnosis. In addition to the cost of treatment, the time away from work can deplete your savings account in no time. Employee coverage options are $10,000 to $40,000 in $10,000 increments. You may elect to cover your spouse and dependent child(ren). Spouse coverage is $10,000 to $40,000 in $10,000 increments (not to exceed 100% of the employee coverage amount) and child(ren) coverage is $5,000 to $20,000 in $5,000 increments (not to exceed 50% of the employee coverage amount).
Hospital Indemnity
Hospital Indemnity insurance is design to help provide financial protection for costs associated with an illness or injury. You can use your hospital indemnity benefits to help cover related expenses like lost income, childcare, deductibles and copays. Benefits are paid directly to you. This plan has a pre-existing condition of 12/12. Any sickness or injury or symptoms for which you received medical treatment, consultation, care or services during the 12 months prior to the effective date will not be covered for a period of 12 months.
Accidental Insurance Rates
Critical Illness Rates
Hospital Indemnity Rates
Sun Life Value Added Benefits
Sun Life offers services and resources that support you in improving your health and making the most of your benefits., Best of all, these are all a part of your benefit plan.
In addition to the core benefits packages offered by TPT, employees can choose to purchase these additional perks for enhanced coverage for themselves and their families.

Pet Insurance
Administered by PetPartners
Pets Are Family and while our bonds with our pets are stronger than ever, rising vet costs create a financial burden that many families struggle with.
Pets eat things they shouldn’t, like their toys or a chocolate bar. Or they may jump off the bed and injure themselves. These unexpected accidents and illnesses can put a dent in your wallet. Pet insurance reimburses you on your pet’s veterinary bills, so you’ll have peace of mind knowing you can care for your pet no matter the cost.
For more information or to enroll, follow these 4 simple steps:
- Click on the "How to Enroll" button (below) or visit the Twin Cities PBS custom website: https://www.petpartners.com/enroll?p=TCPT .
- Enter your pet’s information – name, type, breed, age – and answer 1 medical question. Then enter your zip code and email. Click “Choose Coverage.”
- Customize your plan by selecting the deductible, coinsurance, annual limit and upgrades that fit your pet’s needs. Click “Add to Cart.”
- Enter contact information and billing information. Agree to the terms & conditions. Click “Enroll Now.”
If you want to add more pets, click the “add another pet” button and repeat steps 2 & 3 before clicking “Enroll Now.”
For questions, you can contact PetPartners’, their contact information is included in the resources listed below.
Legal and ID Theft
Administered by Legal Shield | ID Shield
Get comprehensive legal and identity theft protection benefits that are affordable and easy to use. When combined, these plans provide solutions to give you a peace of mind.
LegalShield and IDShield are voluntary insurance policies that are 100% paid by the employees via payroll reductions. Click the links below to learn more!


401(k) Retirement Plan
Administered by Principal
Helping you grow your financial security
Twin Cities PBS offers a 401(k) retirement and savings plan to all employees except those who are considered “Talent.” You will automatically be enrolled in this plan the 1st of the month following 30 days of service unless you opt-out. Employees who do not opt-out will be automatically enrolled at 6%. A yearly increase of 1% is applied until you reach a 15% contribution.
You may contribute up to the maximum allowable by law each year. The contribution limit is $23,500 for 2025, and each year the limit may or may not change. If you are age 50 or older before the end of the year, you may elect to contribute an additional “catch-up” contribution. $7,500 is the 2025 catch-up limit. A matching contribution is made based on the chart. The vesting for the match is automatic at 100%.
Matching Contribution
How do I access, enroll and make changes to my account?
Go online: www.principal.com
Establish your username and password
Enter your SSN and account/contract number 614562
Questions?
Call customer service at (800) 547-7754 or visit www.principal.com
Paid Time Off & Holidays
Administered by Twin Cities PBS
Encouraging Employees to Take Time Off. We understand the importance of time away from the workplace to disconnect enjoy and manage the demands of life.

PTO Accruals
Accruals begin on the first day of employment. Accruals are based on paid hours, excluding overtime. Part-time employees accrue PTO on a pro-rated basis based upon hours worked. PTO does not accrue while an employee is on short-term or long-term disability, TPT-Paid Parenting Leave or unpaid leave. Employees become eligible for the higher accrual rate on the first day of the pay period in which the employee’s anniversary date falls.
The maximum PTO balance that an employee may carry at any time is 200 hours (5 weeks) or the pro-rated equivalent for part-time staff. Once an employee’s PTO balance reaches the maximum, accruals will stop until the employee uses PTO.
Holidays

Elective Programs
Administered by Twin Cities PBS
TPT Membership
Become a member and support TPT's (and your) mission to harness the power of media for the public good! Your donation comes with these benefits: TPT Magazine, our monthly program guide; discounts at retailers and entertainment venues; plus receive free streaming with TPT Passport, unlocking all the shows on the PBS app! It only takes a couple minutes to give at https://e.tpt.org/employees
Contact Us
Sarah Schnell | Vice President of Human Resources
651.229.1277 | sschnell@tpt.org
Denise Jimenez | HR & Benefits Coordinator
phone 651.229.1438 | Djimenez@tpt.org